Prosthetic management of unilateral transradial amputation and limb deficiency: Consensus clinical standards of care
Journal
Journal of Rehabilitation and Assistive Technologies Engineering
Read Online
Authors
Erin O’Brien1, Phillip M Stevens1,2, Steve Mandacina3, Craig Jackman3
- Hanger Institute for Clinical Research and Education, Hanger Inc, Austin, TX, USA
- Division of Physical Medicine and Rehabilitation, University of Utah Health, Salt Lake City, UT, USA
- Upper Limb Prosthetic Program, Hanger Inc, Austin, TX, USA
Background
Of the estimated 2.2 million Americans projected to be living with amputation in 2020, approximately 16% have had an amputation of the upper extremity.1 For patients with a major amputation (at the wrist or above), this amounted to a projected 41,000 people in the United States, as of 2005.1
Currently, for upper limb prostheses, there is an absence of strong, detailed clinical guidance for the practicing clinician.2,3 Because of the lack of published evidence on the effectiveness of one type of upper limb prosthesis over another and the relative absence of clear indications for use of certain upper limb prosthetic components, clinical decision-making has been largely left up to the discretion of the treating prosthetist. However, the number of prosthetists who have a high level of experience treating the upper limb amputee is small relative to those treating lower limb patients.4
In recent years, the field has begun to develop and publish clinical practice guidelines (CPGs) across a range of care episodes including evidence-based guidelines for prosthetic rehabilitation. In the absence of definitive evidence, expert consensus can supply clinically useful guidance in medicine. Clinical practice guidelines created through consensus processes are likely to become more prevalent within orthotics and prosthetics as additional recommendations are sought out by the field.
Objective
To report upon the use of a Delphi consensus effort to establish CPGs for prosthetic design and terminal device options for individuals with unilateral transradial amputation or limb deficiency.
Design
A three-step modified Delphi method was used to establish consensus.5,6 Finding were compiled through a combination of evidence review and subject matter expertise. The modified Delphi method applied quantitative assessments using a five-point Likert scale to identify areas of consensus, with the opportunity for the respondent to provide comments where initial consensus could not be obtained.
An initial SME panel comprised of eight prosthetists with expertise in upper limb prosthetics generated 40 postulates to be used in the Delphi survey. The focus of the 40 postulates was on the indications, contraindications, and considerations associated with prosthesis type (e.g., body powered vs externally powered) and terminal device type (e.g., hand vs hook vs activity specific device) with regard to individuals with unilateral transradial amputations.
These postulates were reviewed by a larger group of 20 prosthetists and two occupational therapists representing a diverse geographic area and an average of 21 years of experience in the treatment of patients with upper limb amputation or limb deficiency.
Results
FIGURE 1
Round 1
- 40 postulates reviewed, 31 of the 40 postulates reached 80% consensus (77.5%) with a response rate of 19/22 respondents (86.4%)
- Postulates that reached consensus averaged 95.8% agreement, those that failed had an average score of 72.5%
- Moderators reviewed 9 postulates that did not reach consensus and participant feedback, two were removed completely based on comments from the experts
Round 2
- 14 modified postulates reviewed, 11 of the 14 postulates reached the 80% consensus (78.6%) with a response rate of 18/22 respondents (81.8%)
- Postulates that reached consensus averaged 94.4% agreement, those that failed had an average score of 75.9%
- Moderators reviewed 3 postulates that did not reach consensus, two were removed completely
Round 3
- 1 modified postulate reviewed, 1 postulate reached 100% consensus with a response rate of 19/22 respondents (86.4%)
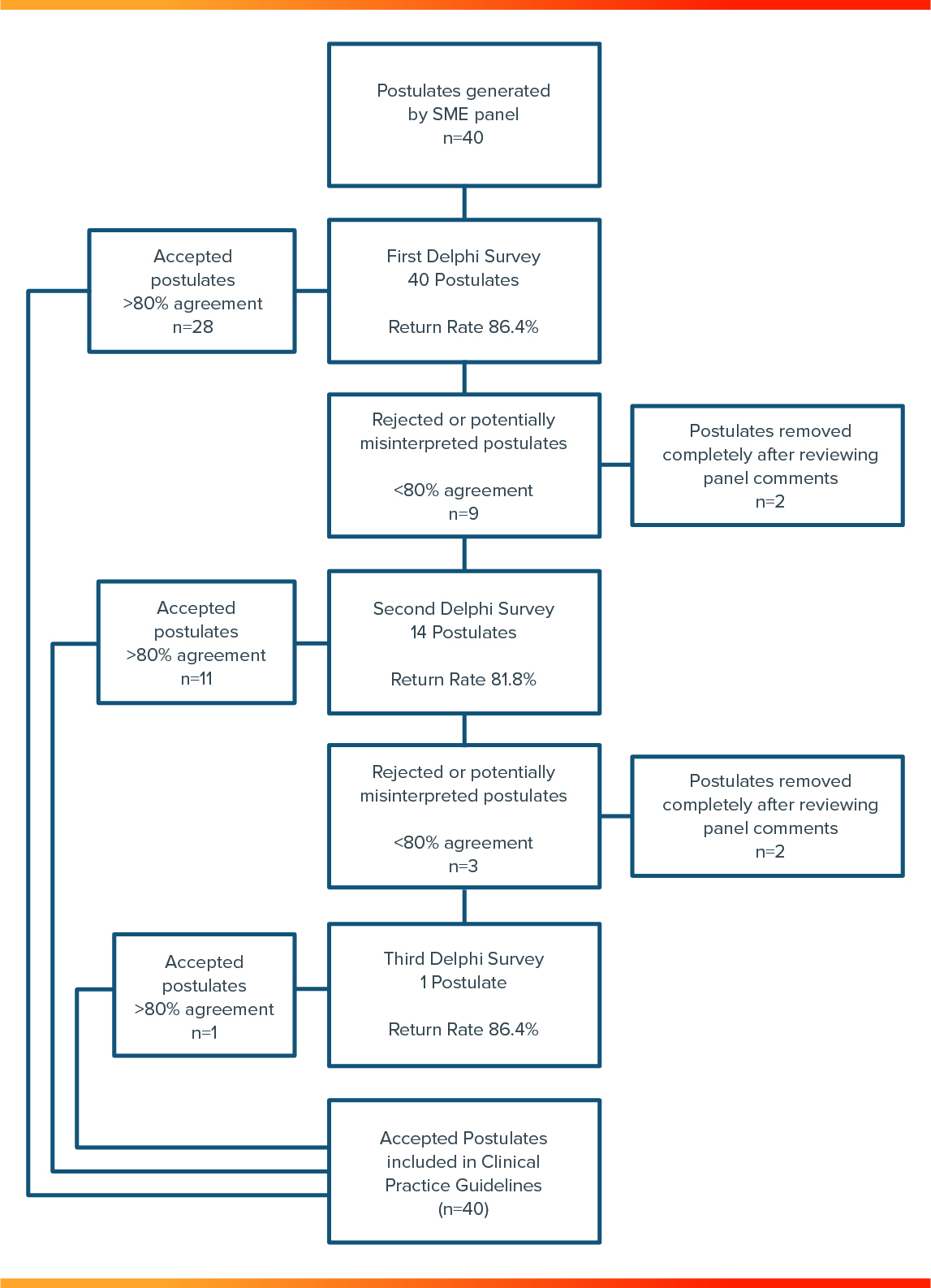
After all three rounds were completed, the statements were grouped according to subject to allow a clinical practice guideline to be written based on the consensus of the group. The 40 individual postulates were combined into nine guidelines that cover a variety of considerations for the unilateral transradial patient (see Appendix A).
Conclusion
- The Delphi process allowed for clinical practice guidelines to be generated for the unilateral transradial amputee in the absence of strong evidence from existing clinical research and literature reviews. By surveying a small group of experts, the process moved quickly and efficiently from item generation through three rounds of surveys to establish a strong set of guidelines for the practicing prosthetist.
- Many prosthetists do not have enough expertise in the area of upper limb prosthetics to allow a high level of confidence in treating this patient population independently. However, with the addition of clinical practice guidelines presented in Appendix A, the decision-making process can be streamlined to help facilitate improved healthcare for this specialized population, while still allowing for individual judgment of the clinician and for the opinion of the patient in determining their care.
Meet the Upper Limb CPG Study Authors




References
[1] Ziegler-Graham, K, MacKenzie, EJ, Ephraim, PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008; 89(3): 422–429.
[2] Carey, SL., Lura, DJ, Highsmith, MJ. Differences in myoelectric and body-powered upper-limb prostheses: systematic literature review. J Rehabil Res Development 2015; 52: 247–262.
[3] Stevens, PM, Highsmith, MJ. Myoelectric and body power, design options for upper-limb prostheses: introduction to the state of the science conference proceedings. J Prosthet Orthot 2017; 29(4s): 1–3.
[4] Uellendahl, J . Myoelectric versus body-powered upper-limb prostheses: a clinical perspective. J Prosthet Orthot 2017; 29(4s): 25–29.
[5] Keeney, S, Hasson, F, McKenna, HP. The Delphi Technique in Nursing and Health Research. Chichester, UK: Wiley-Blackwell, 2011.
[6] Keeney, S, Hasson, F, McKenna, HP. A critical review of the delphi technique as a research methodology for nursing. Int J Nurs Stud 2001; 38(2): 195–200.
More Published Research
The Upper Limb CPG Study is just one of the studies conducted by the Hanger Institute for Clinical Research and Education, in collaboration with leading researchers, clinical, and academic institutions.
Latest Updates
Subscribe to stay up-to-date on our latest posts.


