Microprocessor Feet Improve Prosthetic Mobility and Physical Function
Journal
Journal of Rehabilitation and Assistive Technologies Engineering
READ ONLINE
Authors
Eric L Weber1, Phillip M Stevens1,2, Dwiesha L England1, Vahness D Swilley1 and Shane R Wurdeman1,3
- Hanger Institute for Clinical Research and Education, Hanger Inc, Austin, TX, USA
- Department of Physical Medicine and Rehabilitation, University of Utah Health, Salt Lake City, UT, USA
- Department of Biomechanics, University of Nebraska at Omaha, Omaha, NE, USA
Background
The clinical benefits associated with the microprocessor regulation of prosthetic ankle position and resistance have largely been reported through manufacturer conducted research in controlled laboratory environments. Measures with greater ecological validity are needed. This study is the first to assess physical function and several mobility domains when the only variable to change is the prosthetic foot (socket and suspension remain the same) while transitioning from a non-microprocessor foot to a microprocessor foot.
The primary purpose of this study, conducted by the Hanger Institute for Clinical Research and Education, was to determine the impact of microprocessor feet (MPFs) on physical function among transtibial (below-knee) prosthesis users as they transitioned to the use of a number of commercially available MPFs while maintaining their original socket fit. The secondary aim of this study was to provide preliminary findings on the impact of MPFs on back pain, residual limb pain, and hill ascent and descent.
Objective
To understand if there are differences in physical function and mobility outcomes as patients transitioned from a non-microprocessor to microprocessor feet.
Design
A retrospective analysis of patient outcomes was performed. Patient-reported benefits associated with the adoption of prosthetic foot-ankle mechanisms were collected from 23 individuals throughout the longitudinal use of a custom short form of the Patient-Reported Outcomes Measurement Information System (PROMIS) – Physical Function (PROMIS-PF) and individual items from the Prosthesis Evaluation Questionnaire (PEQ).
Results
Through this retrospective analysis, significant increase in physical function and significant improvements in several mobility items were observed. Collectively, these measures support the beneficial impact of MPFs on improving socket comfort, reducing back pain, improving sit to stand transfers, and enhancing hill ascent and descent as well as stair negotiation.
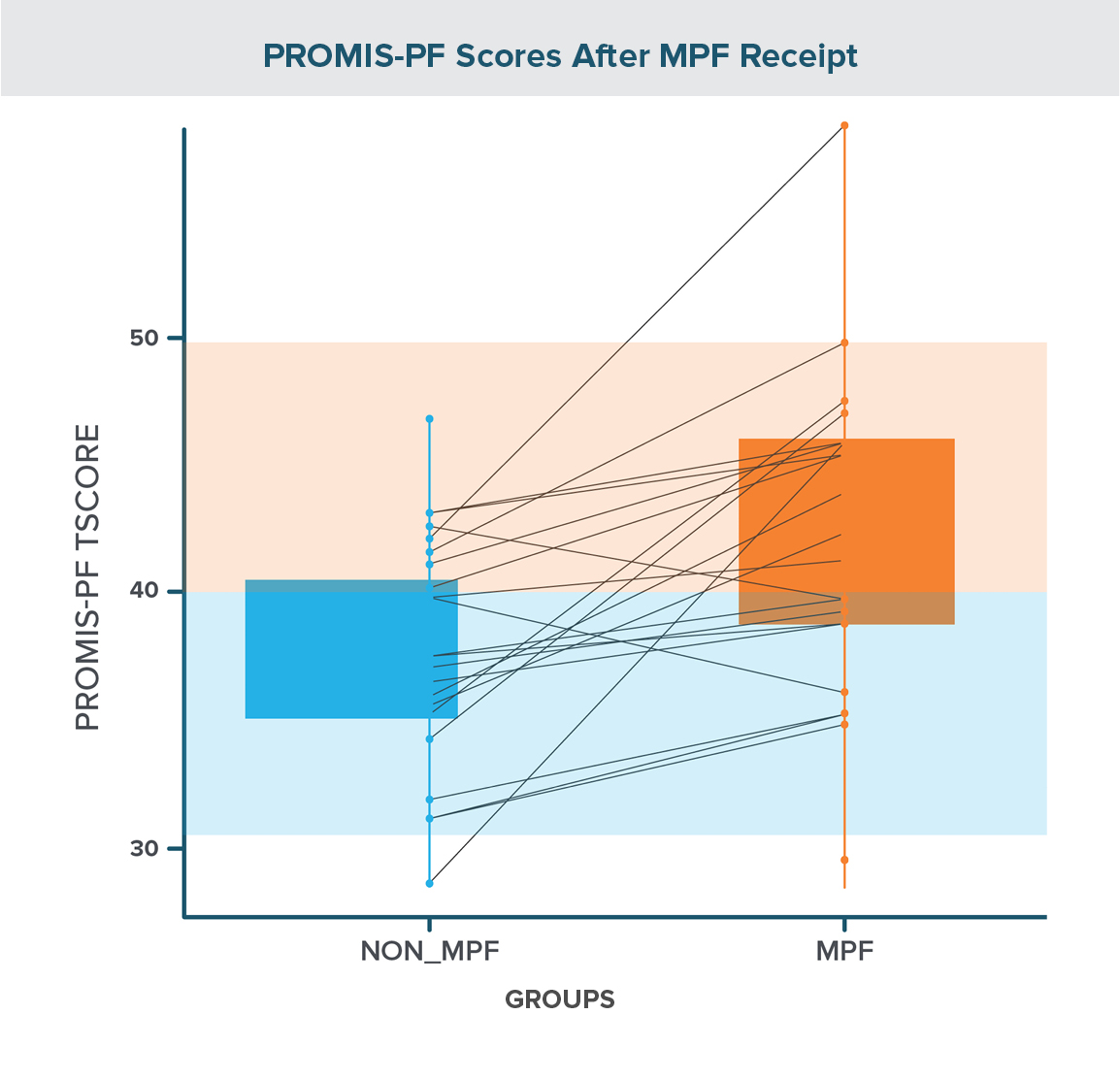
Figure 1
Univariate analysis
Using a paired t-test for analysis, there was a significant increase in PROMIS-PF scores with the use of a MPF compared to those observed with the non-MPF (MPF – non-MPF mean difference: 5.40 ± 1.25; t(19) = 4.31 (p = 0.0004).
Multivariate analysis
A similar finding was noted with the multivariate analysis. When controlling for confounders, such as age, gender, etiology, and time between assessment, individuals’ PROMIS-PF T-Scores increased by 5.40 points (95% CI [2.88-7.91], χ2 (1) =13.64, p = .0002).
Prosthesis evaluation questionnaire
With respect to general directionality, all queried items from the PEQ improved with the transition from a non-MPF to a MPF. With respect to the perceived quality of the socket fit, significant improvements were noted with respect to both prosthesis fit (p = .035) and sitting comfort with the prosthesis (p < .001). Improvements with respect to the intensity of back pain were statistically significant (p = .010). Significant improvements were observed for both ascent (p < .001) and descent (p < .001) of steep hills in the MPF conditions.
Conclusion
This study supports previous findings conducted in controlled laboratory walking environments showing benefits associated with MPFs, including:
- Improved biomechanical performance during the negotiation of ramps and stairs;
- Increased toe clearance in swing; and
- Reduced peak pressures against the residual limb within the socket and increased prosthetic mobility.
Additionally, this study demonstrates how MPFs interact outside of the laboratory when the only prosthetic variable was the transition from non-MPFs to MPFs. Prosthesis users who transitioned from non-MPFs to MPFs experienced a significant improvement in their physical function score as measured by the PROMIS-PF. In addition, socket comfort, back pain, residual limb pain, and hill ascent and descent showed improved scores from the independent items taken from the PEQ.
Meet the Authors




Vahness Swilley
Director of Operations, Clinical & Scientific Affairs

More Published Research
This publication is just one of the studies conducted by the Hanger Institute for Clinical Research and Education, in collaboration with leading researchers, clinical, and academic institutions.
Latest Updates
Subscribe to stay up-to-date on our latest posts.


