Advancing Our Understanding of the Impact of Prosthetic Foot Design

Of the 1.6 million people living with limb loss in the United States, approximately 1.3 million (86%) have an amputation of the lower limb.1,2 The prosthetic foot is an integral component of any lower limb prosthesis after major lower limb amputation (i.e., ankle disarticulation level or proximal) due to its proven impact on function, mobility, and quality of life. A range of prosthetic foot designs have been developed over the years to reflect the evolving demographics of the amputee population, allowing for the appropriate pairing of prosthetic foot type to the individual end user.
The Principles of Prosthetic Foot Design
One of the foundational principles observed in prosthetic feet is that of energy storage and return (ESAR). The concept, introduced over 30 years ago, represents the reality that when certain materials deform under load, they will return to their original shape the moment they are able to, releasing a portion of the energy that created the original deformation. In practical terms, when a prosthesis user rolls onto the ball of their prosthetic foot, their weight and momentum will cause the foot to bend. As they shift their weight to their other limb, the foot is able to return to its original shape, mimicking the “push-off” that occurs in standard walking and propelling the leg forward.
Early research on ESAR feet was largely performed on younger, healthy subjects with no overlapping comorbid health conditions, such as diabetes or dysvascular disease. However, in the decades that followed, the demographics of the amputee population shifted to a larger representation of older patients with amputations secondary to metabolic disease processes. As this shift has occurred, it has led policy makers to question whether the principles of ESAR still apply within older users of lower limb prostheses.
The question suggests the overgeneralization that older users with comorbid health conditions are incapable of sustained ambulation and elevated speeds. However, to the extent that such users walk aggressively enough to deform their prosthetic feet, or take enough steps to benefit from the protective properties that propulsion can provide to the rest of the body, then the principles of ESAR should be made available to this target population
The Impact of ESAR Feet in Today’s World
In an effort to better understand the significance of prosthetic foot design on current users, including the older population and those with diabetes or dysvascular disease, the Hanger Institute for Clinical Research and Education recently completed various clinical studies examining foot design as a meaningful consideration for lower limb prosthesis users.
Older patients with amputations secondary to the consequences of metabolic disease benefit from the use of ESAR feet provided they have the physical capacity to walk at elevated walking speeds.3
Mobility Analysis of AmpuTees (MAAT) 5
The MAAT 5 study examined the prosthetic mobility observed among elderly prosthesis users with amputations due to diabetes or dysvascular disease across a range of commonly worn ESAR feet. We retrospectively identified nearly 900 subjects that met our inclusion criteria. After controlling for extraneous variables, our data confirmed that users of ESAR feet reported reasonably high prosthetic mobility levels.
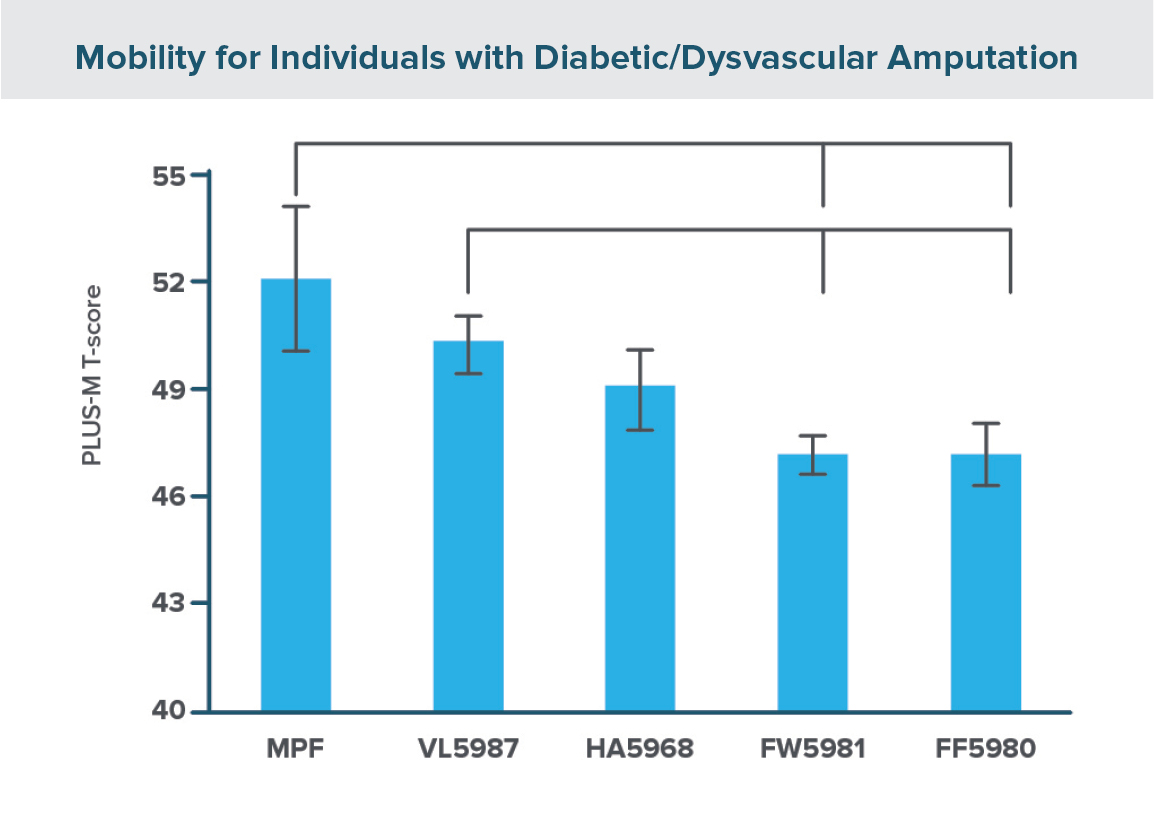
In addition to observing high mobility scores across all ESAR foot types, we observed a steady increase in prosthetic mobility with progressively advanced prosthetic foot design, with the lowest scores observed with the most basic ESAR feet, often described as “Flex-Foot” (L5980) and “Flex-Walk” (L5981).
Advanced ESAR Foot Designs
- Users of an ESAR foot with a hydraulic ankle mechanism (L5968) reported higher average prosthetic mobility levels.
- Even higher mobility was associated with those users fit with ESAR feet with vertical shock absorption properties (L5987).
- The highest mobility levels were observed among those subjects using ESAR feet with microprocessor control of hydraulic ankle mechanisms (MPF feet).
This data suggests that the selection of a prosthetic ankle-foot type directly impacts functional mobility for patients with an amputation due to diabetes and/or vascular disease and lays a foundation for further research as we continue to better understand the relationship between prosthetic foot design and a patient’s prosthetic mobility.
Shock absorbing feet are consistently associated with enhanced prosthetic mobility irrespective of whether this biomechanical behavior is the result of a distinct mechanical device or the manipulation of material science and design geometry.4
Outcomes ASsessment and DISsemination (OASIS) 2
During a recent reimbursement coding review, several prosthetic feet that were historically coded with the shock-attenuating function were assigned new billing codes. National policy makers suggested that these prosthetic feet required distinct shock absorbing mechanical features to retain their historical coding, and that similar benefits could not be obtained through creative manipulation of material science and geometry.
This position conflicted with clinical observation, so through OASIS 2 we sought to assess the position by monitoring the prosthetic mobility levels reported by over 500 users of ESAR feet with shock absorption through design engineering, ESAR feet with shock absorption through distinct mechanical features, and basic ESAR feet with no absorptive properties.
Our findings suggested a few important principles. First, the presence of shock absorptive behaviors, whether through engineering or a distinct mechanical feature, is associated with a significant increase in prosthetic mobility relative to basic, non-absorbing ESAR feet.
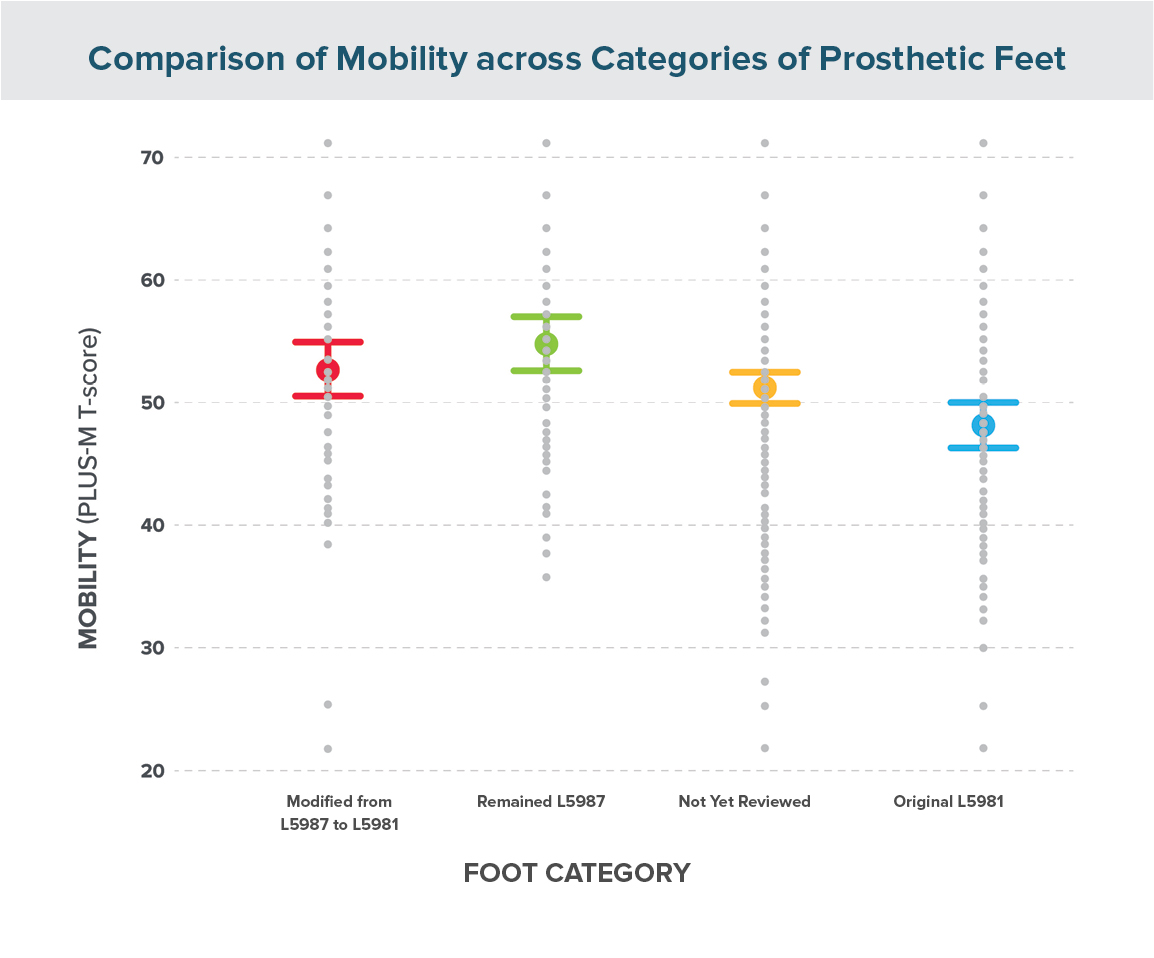
Second, while there was variation in performance among the engineered absorbing feet, some were associated with equivalent prosthetic mobility to that associated with a distinct mechanical feature. Overall, our findings confirmed that focusing on the patient’s functional outcomes over visible features appears to be the pathway towards identifying higher performance, and thus, a possible consideration in reimbursement structure.
Microprocessor feet (MPFs) improve physical function and mobility along with improving socket comfort, reducing back pain, improving sit to stand transfers, and enhancing hill ascent and descent, as well as stair negotiation.5
Impact of Microprocessor Feet vs. Non-Microprocessor Feet on Mobility and Function
In 2022, we published a study that examined the performance characteristics associated with MPFs. In contrast to the previously described studies where we examined a large cross-sectional cohort to confirm expected correlations, we followed a smaller sample through a longitudinal cross-over design. We identified 20 patients currently using non-articulating ESAR feet and tracked a series of outcomes as they transitioned into an MPF while the other elements of their prosthesis (interface, socket, suspension) remained constant.
We assessed mobility using a custom short-form of the PROMIS physical function survey. This approach allowed us to compare the physical function experienced by the prosthesis users against that reported by the general US population. In creating the custom short form, we selected items that we anticipated might be sensitive to a change in foot design such as sit to stand transfers, walking, and navigating stairs.
Our findings confirmed the potential of MPFs to enhance physical function in a meaningful way. In their baseline ESAR foot, our subjects reported a physical function that was more than one standard deviation below that of the mean value of the general population. In transitioning to the MPF, the associated improvements reported by our subjects were not only statistically significant, but also exceeded the minimum clinical important difference (MCID) for the measure, suggesting a clinically meaningful improvement with their MPF.
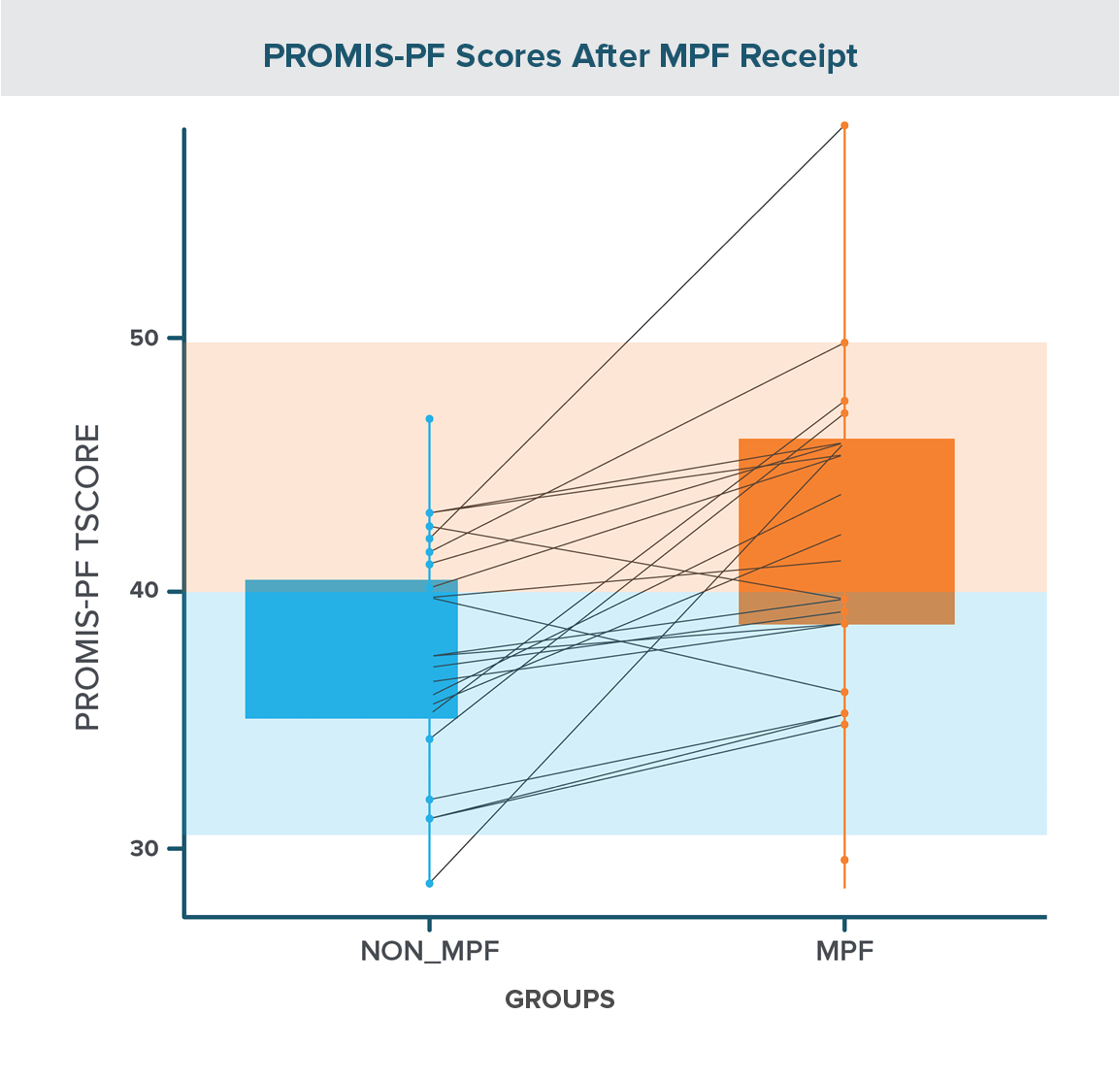
Further, their mean physical function score was now within a single standard deviation of the population mean. A sub-analysis of individual items suggested that the tasks associated with the greatest improvements were sit to stand transfers and navigating ramps and stairs, followed by the ability to bend down to retrieve something from the floor, with only modest benefits associated with the comparatively simple tasks associated with level ground walking.
In addition to mobility, we chose several items from the Prosthesis Evaluation Questionnaire (PEQ) that would provide us with a more holistic view of the impacts of the change in foot design. The areas of greatest improvement with the use of MPFs were in environmental mobility, with significant improvements in hill ascent and descent. Also noteworthy was a significant improvement in socket fit and comfort, even though the socket itself did not change. This improvement reflects the ability of MPFs to beneficially alter the loading forces experienced within the prosthetic socket. A final notable observation was a significant reduction in low-back pain with the use of MPFs.
Conclusions
While our efforts to improve our understanding of the impact of foot design on the well-being and function of prosthesis users will continue, these studies support the idea that prosthetic foot selection significantly impacts patient outcomes. Key findings that should be reflected in the policy statements of health insurance coverage considerations, include:
- Older patients with amputations secondary to the consequences of metabolic disease benefit from the use of ESAR feet, provided they have the physical capacity to walk at elevated walking speeds.
- Shock absorbing feet are consistently associated with enhanced prosthetic mobility, irrespective of whether this biomechanical behavior is the result of a distinct mechanical device or the manipulation of material science and design geometry.
- Microprocessor feet appear to facilitate meaningful improvements in physical function, especially with respect to transfers and the navigation of environmental obstacles. Furthermore, they are also associated with reduced pain levels in both the residual limb and lower back.
Collectively, we can continue to assert that foot design is an extremely meaningful consideration for users of lower limb prostheses and future patient protocols.
More Published Research
Review additional studies conducted by the Hanger Institute for Clinical Research and Education, in collaboration with leading researchers, clinical, and academic institutions.
1. Dillingham T, Pezzin L, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J 2002;95:875–883.
2. Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008; 89: 422–429.
3. Wurdeman SR, Stevens PM, Campbell JH. Mobility analysis of AmpuTees (MAAT 5): Impact of five common prosthetic ankle-foot categories for individuals with diabetic/dysvascular amputation. Journal of Rehabilitation and Assistive Technologies Engineering. 2019 Feb;6:2055668318820784.
4. Miller TA, Campbell JH, England DL, Stevens PM, Wurdeman SR. OASIS 2: Mobility differences with specific prosthetic feet across procedure codes. Journal of Rehabilitation and Assistive Technologies Engineering. 2022 May 8;9:20556683221101623.
5. Weber EL, Stevens PM, England DL, Swilley VD, Wurdeman SR. Microprocessor feet improve prosthetic mobility and physical function relative to non-microprocessor feet. Journal of Rehabilitation and Assistive Technologies Engineering. 2022 Jun 30;9:20556683221113320.
Latest Updates
Subscribe to stay up-to-date on our latest posts.