Landmark Clinical Trial Finds Microprocessor Knees Improve Safety and Preserve Quality of Life for Older Prosthesis Users
Journal
Disability and Rehabilitation
READ ONLINE
Authors
Shane R. Wurdeman1, Brian J. Hafner2, Andrew Sawers3, Dwiesha L. England1, Russell Lundstrom4, Andreas Kannenberg 4
- Hanger Institute for Clinical Research and Education, Austin, Texas, United States of America.
- Department of Rehabilitation Medicine, University of Washington, Seattle, WA, USA.
- Department of Kinesiology and Nutrition, University of Illinois Chicago, Chicago, IL, USA.
- Department of Clinical Research and Services, Otto Bock HealthCare LP, Austin, TX, USA.
Background
Falls can be life-altering, especially for individuals of advanced age and/or those that have difficulty with their mobility. This is especially true for patients with an above-knee amputation. Traditionally, individuals with an above-knee amputation that were classified as limited community ambulators (Medicare K2 level) were largely limited to non-microprocessor knee (NMPK) options.
However, advancements in science and policy have brought a welcomed expansion to the options that can be considered for this population, including microprocessor knees (MPKs) where appropriate. The advent of MPKs introduced technology capable of responding to real-time gait changes, offering enhanced stability, stumble recovery, and improved user function.
Clinical practice guidelines now recommend MPKs over NMPKs to support safer ambulation and greater user satisfaction. MPKs have demonstrated benefits including reduced fall risk, improved mobility on uneven terrain, lower energy expenditure, and higher health-related quality-of-life (HR-QoL). However, despite these advantages, individuals classified as K2—especially those aged 65 and older—have historically had limited access to MPKs. These individuals exhibit elevated fall risk and a higher prevalence of activity avoidance due to fear of falling.
The field has been accumulating evidence of the benefits of MPKs for K2 patients for many years. However, there were continued pressures to demonstrate benefits through a large two-arm randomized, controlled trial.
The ASCENT K2 study examined the long-term impact of MPKs versus NMPKs in K2-level prosthesis users aged 65 and older. This 12-month prospective randomized, controlled trial assessed how prosthetic knee type influenced fall events, activity avoidance behaviors, and associated outcomes such as HR-QoL, mobility, and balance confidence. Results showed that individuals using MPKs experienced significantly fewer falls and near-falls, and reported less activity avoidance due to fear of falling, compared to those using NMPKs. Participants in the MPK group also maintained their HR-QoL, while those in the NMPK group experienced a significant decline.
Objective
To assess the effects of MPKs versus NMPKs among unilateral, above-the-knee prosthesis users classified as Medicare K2 ambulators over the age 65.
Design
A two-arm, 12-month randomized controlled trial to compare MPKs to standard-of-care NMPKs. Fear-of-falling avoidance behavior (FFABQ), falls and near-falls were assessed alongside additional measures of mobility, balance, and health-related quality-of-life (HR-QoL).
Results
A total of 107 individuals were enrolled. At the conclusion of the 12 months, individuals randomized to the MPK reported approximately one fall compared to individuals randomized to the NMPK who reported approximately three falls. Further, those randomized to the MPK reported approximately two near-falls compared to approximately six near-falls in the NMPK cohort. When these two measures were aggregated, individuals that were provided an MPK had significantly fewer fall events compared to those with the NMPK. Results were significantly favorable for mobility and HR-QoL for the MPK group and not the NMPK group.
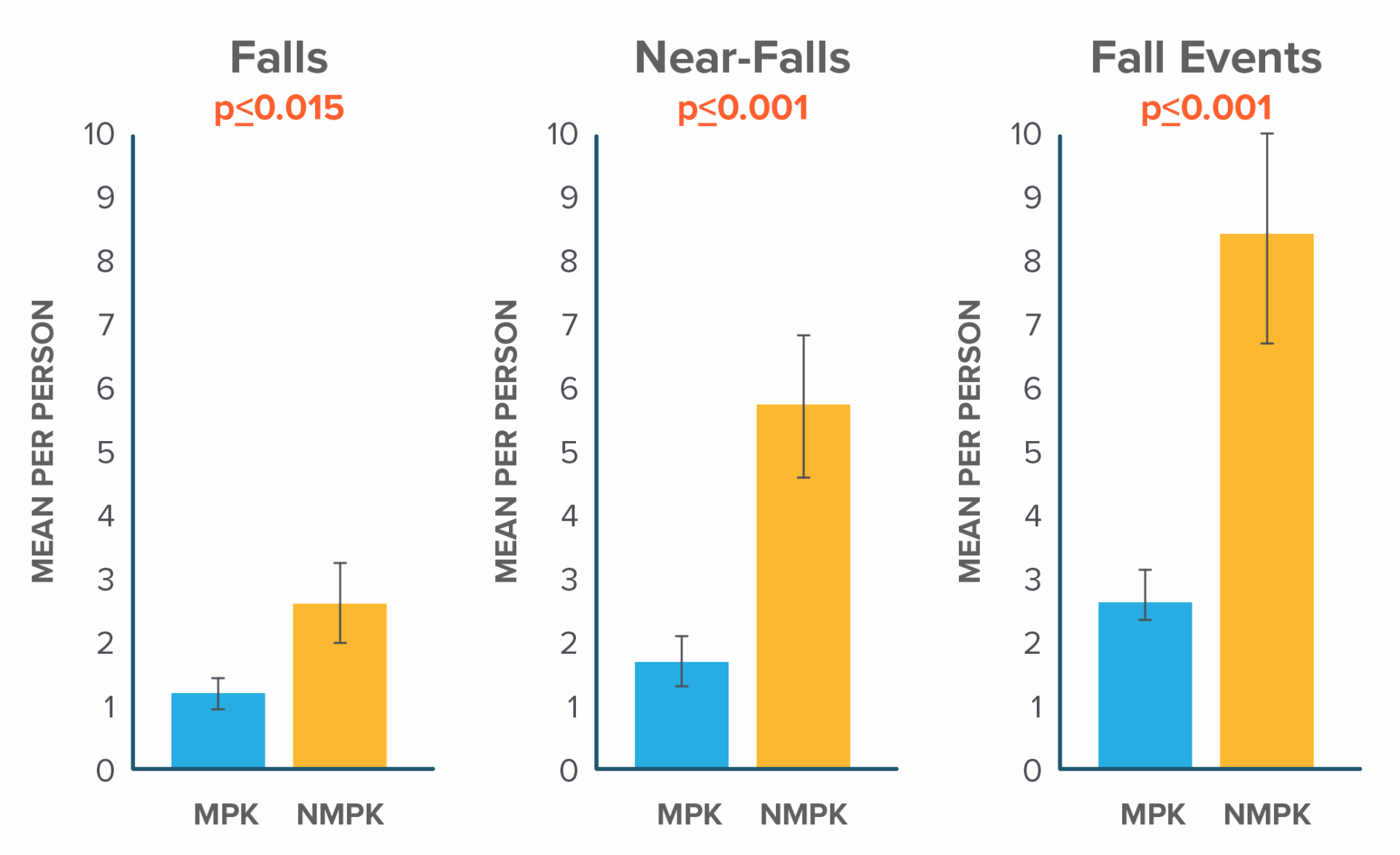
Figure 1
Significant reduction in patient self-reported fear of falling and avoidance behaviors (as measured by the FFABQ) and faster Timed Up and Go scores (by approximately 10 seconds) were also observed.
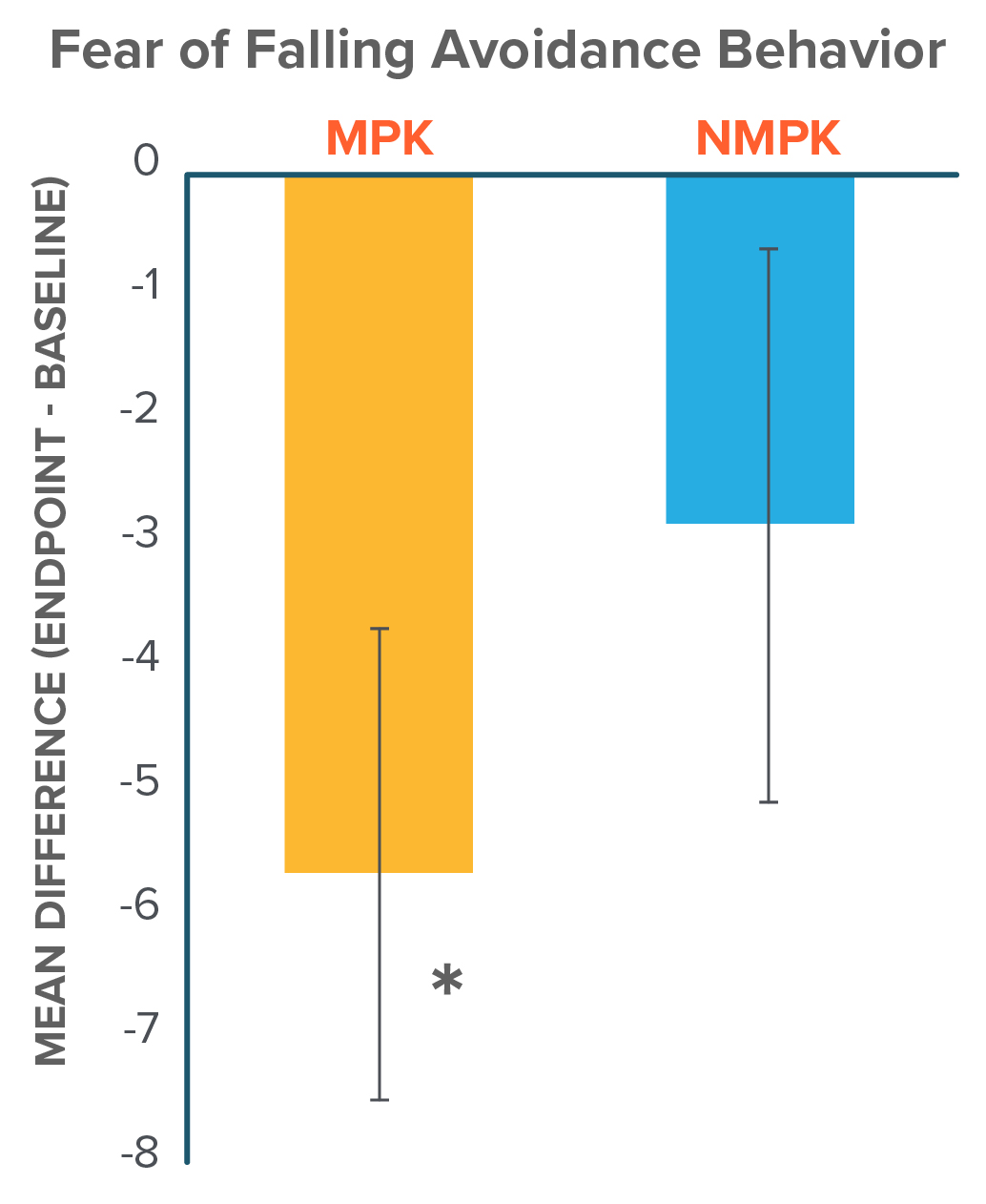
Figure 2
Participants in the MPK group demonstrated a significantly decreased (i.e. improved) score on the FFABQ, while the nMPK group demonstrated no significant changes over the 12-month trial period. *p < 0.05
Conclusion
- The ASCENT K2 clinical trial found that individuals over 65 with above-knee amputations and limited mobility (K2 level) experienced significantly fewer falls and near-falls when using MPKs compared to NMPKs—reporting about one-third as many fall-related events.
- MPKs resulted in lower levels of activity avoidance due to fear-of-falling and better HR-QoL as opposed to NMPKs.
- Expanded use of MPKs has the potential to enhance safety and HR-QoL among older prosthesis users with limited functional capabilities.
- This evidence, paired with recently announced policy changes from the Centers for Medicare & Medicaid Services (CMS), provides a foundation for the identification of appropriate K2 prosthetic candidates for MPKs and the reasonably expected benefits attached to that treatment plan.
More Published Research
This publication is just one of the studies conducted by the Hanger Institute for Clinical Research and Education, in collaboration with leading researchers, clinical, and academic institutions.
Latest Updates
Subscribe to stay up-to-date on our latest posts.


