Mobility Analysis of AmpuTees II (MAAT II): Comorbidities and Mobility in Lower Limb Prosthesis Users
Journal
American Journal of Physical Medicine & Rehabilitation
READ ONLINE
DOWNLOAD ONLINE
Authors
Shane R. Wurdeman, PhD, CP, FAAOP(D)1,2, Phillip M. Stevens, MEd, CPO, FAAOP1,3, James H. Campbell, PhD, CO, FAAOP1
- Department of Clinical and Scientific Affairs, Hanger Clinic, Austin, TX
- Department of Biomechanics, University of Nebraska at Omaha, Omaha, NE
- School of Medicine, University of Utah, Salt Lake City, UT
Background
As the prevalence of lower limb loss in the United States increases, the importance of ensuring patient access to prosthetic rehabilitation continues to rise. The characterization of patients with lower limb amputation and their expected function with prosthetic technology is critical for appropriate resource allocation. Comorbidities represent a facet of overall health that may identify patient populations that require additional consideration in the development of a prosthetic treatment plan.
The goal of this study was to analyze the impact of comorbid health concerns on mobility in patients with lower limb prostheses. This investigation will help optimize treatment plans and resource allocations.
Objective
To identify comorbidities that may be significant predictors for decreased mobility, as well as uncover the role comorbid health may play in the mobility realized by lower limb prosthesis users.
Design
The study consisted of a database chart review, with patients grouped according to comorbidities. A convenience sample of 596 patients seen nationally in clinics were confirmed to have one or more comorbid health conditions. Patient mobility was assessed as the T-scores taken from the Prosthetic Limb Users Survey of Mobility (PLUS-M), a patient-reported outcome measure assessing the relative difficulty associated with a range of routine mobility tasks. Regression models were used to determine those comorbidities that acted as significant predictors of reduced mobility levels. A general linear univariate model was also used to explore differences in mobility among those cohorts. Common comorbidities included diabetes, peripheral vascular disease (PVD), heart disease, forms of arthritis, upper gastrointestinal disease, depression, anxiety, degenerative disc disease, and obesity.
Results
Of the 18 queried comorbidities and demographic considerations, the only presentations found to have a significant effect on the mobility of lower limb prosthesis users were an age over 65 year old, history of stroke, the presence of PVD, and a history of anxiety or panic disorders. Of these, only a positive history of stroke and anxiety or panic disorders were associated in mobility deficits large enough to be considered clinically significant. When the four variables cited above were removed from consideration, there were no significant differences in prosthetic mobility between groups with no comorbid health conditions and those with multiple, increasingly layered comorbid health states.
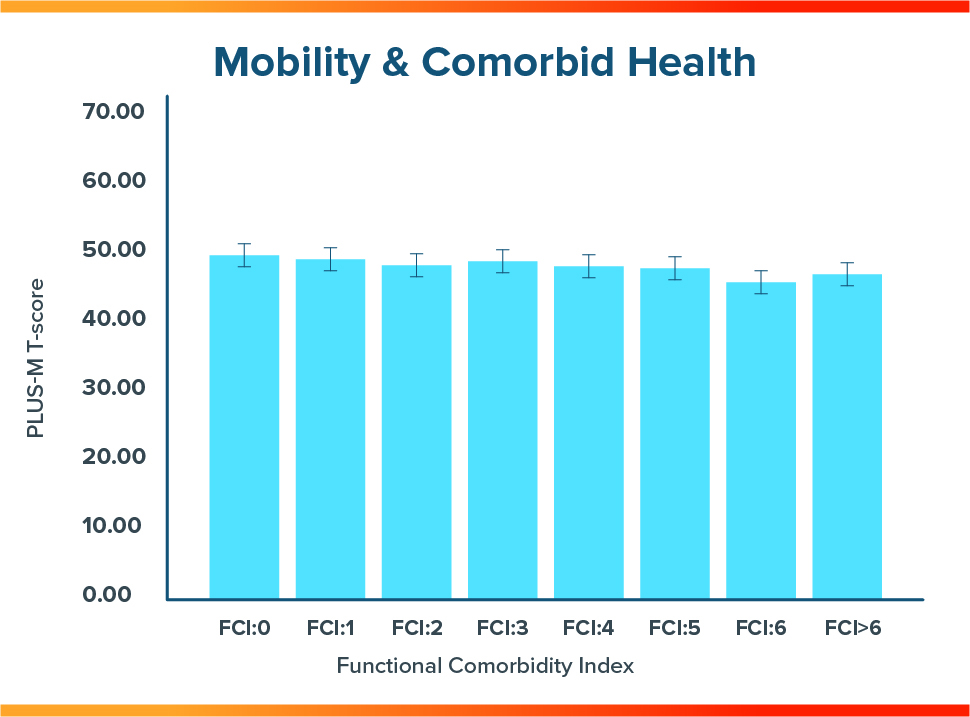
Conclusion
- Patients with a history of stroke or anxiety/panic disorders should be examined with care as part of the rehabilitation plan for optimizing future mobility.
- Diabetes was not a significant factor for lower limb prosthesis users’ mobility.
- In general, a patient’s overall comorbid health is not a factor for the patient’s mobility with a lower limb prosthesis.
Meet the Authors



More Published Research
This publication is just one of the studies conducted by the Hanger Institute for Clinical Research and Education, in collaboration with leading researchers, clinical, and academic institutions.
Latest Updates
Subscribe to stay up-to-date on our latest posts.