Development and Initial Validation of the Orthotic Patient-Reported Outcomes – Mobility (OPRO-M): An Item Bank for Evaluating Mobility of People Who Use Lower-Limb Orthoses
Journal
PloS One
READ ONLINE
Authors
Geoffrey Balkman1, Alyssa Bamer1, Phillip Stevens2,3, Eric Weber2, Sara Morgan1,4,5, Rana Salem1, Dagmar Amtmann1, Brian Hafner1
- Department of Rehabilitation Medicine, University of Washington, Seattle, Washington, United States of America.
- Hanger Institute for Clinical Research and Education, Austin, Texas, United States of America.
- Department of Physical Medicine and Rehabilitation, University of Utah, Salt Lake City, Utah, United States of America.
- Gillette Children’s Specialty Healthcare, St. Paul, Minnesota, United States of America.
- University of Minnesota, Minneapolis, Minnesota, United States of America.
Background
Lower limb orthoses (LLOs) are external leg braces designed to improve or maintain mobility in individuals with a variety of conditions affecting lower limb function. Despite the recognized benefits of LLOs, orthotists infrequently evaluate their effectiveness by measuring patients’ mobility outcomes.1,2 In a prior study, orthotists reported that time constraints and the lack of instruments designed for LLO users were major barriers to routine outcomes measurement.2
Patient-reported outcome measures (PROMs) can provide insights into important aspects of a LLO user’s mobility and help clincians assess the effectiveness of orthoses. This study conducted by the Hanger Institute for Clinical Research and Education and the University of Washington aimed to create a population-specific item bank for measuring the mobility of LLO users. The resulting questionnaire, the Orthotic Patient-Reported Outcomes—Mobility (OPRO-M), was evaluated for convergent, divergent, and known groups’ construct validity. The OPRO-M was also found to correlate strongly with existing PROMs designed to measure aspects of physical function.
Results from this study indicate that OPRO-M can effectively measure the mobility of LLO users. This illustrates the opportunity to successfully quantify clinical intervention and identify where possible improvements can be made. As a result, several versions of the instrument are now available to the field to incorporate into clinical practice and research studies.
Objective
To develop an outcome measure relevant to LLO users and evaluate its validity.
Design
A cross-sectional survey was administered to a national sample of LLO users. Participants responded to questions about their mobility, health, orthosis use, and demographics. Responses to candidate questions for the new outcome measure were analyzed to create a set of questions that evaluate a wide range of mobility.
Results
Responses were collected from 1,039 lower limb orthosis users. A total of 39 questions were found to be unidimensional, indicating that they measure a single primary trait (i.e., mobility) with minimal redundancy. There was no evidence of floor or ceiling effects, suggesting that few LLO users will receive scores at the lowest or highest extremes of the measurement scale. Additionally, the OPRO-M items showed no significant differential item functioning (DIF), suggesting the tool measures mobility in LLO users without bias from variables generally unrelated to mobility. Strong positive correlations were observed between OPRO-M scores and scores from comparison questionnaires applicable to lower limb orthosis users. A 20- and 12-item short form were created for efficient administration.
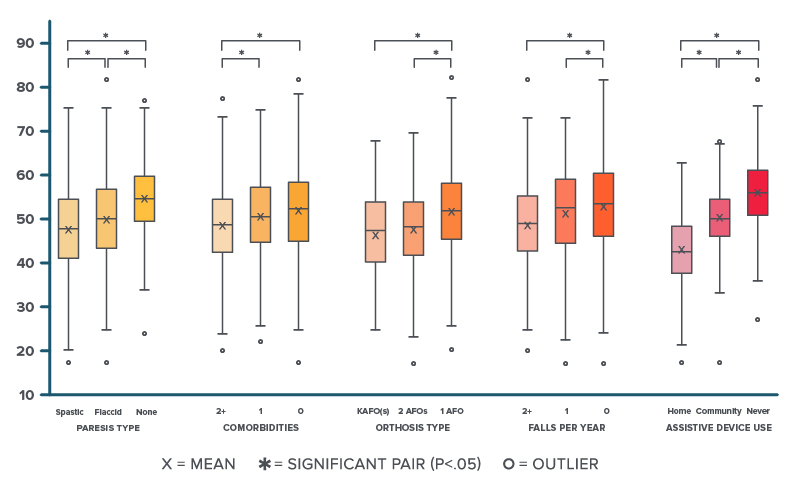
Evaluation of Known Groups’ Construct Validity
ANOVA (Analysis of Variance) is a statistical test used to compare means across multiple groups. One-way ANOVA testing revealed that there were statistically significant differences in OPRO-M full bank T-scores, between at least two groups for all characteristics, including orthosis level (F(2, 2) = [25.08], p < 0.001), paresis type (F(2, 2) = [27.59], p < 0.001), assistive device use (F(2, 2) = [286.45], p < 0.001), fewer falls in the prior 12 months (F(2, 2) = [15.02], p < 0.001) and number of comorbidities (F(2, 2) = [7.08], p < 0.001).
Conclusion
OPRO-M is a versatile patient-reported outcome measure designed to evaluate the mobility of LLO users. This new questionnaire includes activities and situations relevant to using lower limb orthoses, and can be administered efficiently in a clinical setting. OPRO-M scores may help identify the functional impact lower limb orthoses have on the individuals who use them.
Additionally, OPRO-M:
- Focuses on aspects of mobility that are most relevant to lower limb orthosis users.
- Can be used to communicate with patients about how their mobility changes with the use of their orthoses.
- Offers the potential to measure the effectiveness of clinical interventions and identify areas for enhancement.
- May be used to support the medical necessity of LLOs.
More Published Research
This publication is just one of the studies conducted by the Hanger Institute for Clinical Research and Education, in collaboration with leading researchers, clinical, and academic institutions.
1. Robinson, C., & Fatone, S. (2013). You’ve heard about outcome measures, so how do you use them? Integrating clinically relevant outcome measures in orthotic management of stroke. Prosthetics and orthotics international, 37(1), 30–42. https://doi.org/10.1177/0309364612446650
2. Hall, N., Parker, D., & Williams, A. (2020). An exploratory qualitative study of health professional perspectives on clinical outcomes in UK orthotic practice. Journal of foot and ankle research, 13(1), 49. https://doi.org/10.1186/s13047-020-00416-w
Latest Updates
Subscribe to stay up-to-date on our latest posts.


