A Professional Overview: Identification and Treatment of Toe Walking

Idiopathic toe walking (ITW) is the diagnosis given to children who walk on the balls of their feet or their toes when all other medical diagnoses have been ruled out. Oftentimes, parents believe their children will just grow out of it. This is most often not the case. Once idiopathic toe walking has been identified, it is important to start treatment immediately to minimize time in treatment and work towards typical gait patterns. Hanger Clinic Pediatric Specialist Gwen Ansier, CO, shares with us a professional overview of identifying and treating toe walking.
Identifying/Diagnosing Toe Walking
Toe Walking is a stance phase issue and is defined as the failure of the heel to contact the floor at the onset of stance during the gait cycle. Idiopathic Toe Walking (ITW) refers to the manifestation of this gait pattern without a known underlying pathological cause. This is a diagnosis of exclusion, in which other conditions have been ruled out.
Other gait kinematic abnormalities that are associated with toe walking include:
- Early firing of the gastrocnemius with absent heel strike
- Lack of knee extension
- Present knee hyperextension
In typically developing children, consistent heel strike during initial stance occurs by 15-18 months of age or around five and a half months after the onset of independent walking. All gait characteristics should be mature by age five.
Idiopathic Toe Walking will always exhibit bilateral and symmetrical presentation, as opposed to some other neurologic conditions which may cause unilateral or asymmetric toe walking.
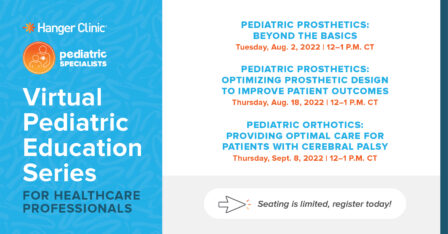
Pediatric Education Series
Join Hanger Clinic Pediatric Specialists from around the country to continue learning about orthotic and prosthetic solutions for your pediatric patients. The courses in this series are virtual and free of charge.
Disorders and Toe Walking
It is important to first take into account any potential underlying causes for toe walking. Vision, gastrointestinal (GI), or sensory issues can all play a role in the child developing a toe walking gait pattern. Toe walking can also be associated with neuromuscular or musculoskeletal conditions. Toe walking may be caused by Cerebral Palsy, congenital contracture of the Achilles tendon, or paralytic muscular disorders such as Duchenne Muscular Dystrophy. Idiopathic Toe Walking may be associated with developmental disorders such as Autism or other myopathic or neuropathic disorders.2
Other common contributing factors for toe walking include:
- Prematurity
- Refluxes and GI Issues
- Torticollis
- Congenital Contracture
- Vision Issues
- Sensory Processing Disorder
- Autism Spectrum Disorder (ASD)
A study by Sobel et al revealed that the majority of child who present with Idiopathic Toe Walking had a normal birth weight, walked on time, began to toe walk immediately in their gait development, stood mostly in plantigrade (feet flat), were able to demonstrate heel-toe gait when instructed, and only toe walk intermittently.
Consequences of Toe Walking
Consequences of toe walking can be severe; after months and/or years of toe walking an acquired contracture of gastrocnemius and soleus can occur. Children with excessive toe walking often present with excessive external rotation and external tibial torsion to accommodate for their plantar flexion contracture. Even after successful treatment of toe walking, some children will be left with this external rotation or torsional deformities. Furthermore, a number of sensory toe walkers prefer to externally rotate their hips to give a different sensory input while walking. De-rotation straps can be used to help with position and strengthening, though straps will be ineffective once rotational boney deformity has occurred. The earlier intervention is started, the fewer deformities, pain, and abnormalities for the child.
If left untreated, toe walking is associated with:
- Muscle contractures
- Widening forefoot
- Poor alignment
- Pain in feet, ankle, knees, and back
Assessment
When treating toe-walking patients, it is most important to have three sections incorporated into the evaluation.
- Patient history
- Physical examination
- Gait analysis with video recording
When obtaining patient history, the clinician is responsible for obtaining all information pertinent to development and possible associated causes, noting any additional services needed to help treat the gait abnormality. The physical examination should consist of a thorough range of motion assessment, spasticity screening, and determining the percentage of time the patient ambulates with a toe walking gait pattern. Lastly, video gait analysis of the patient ambulating both with and without footwear is necessary to have a full assessment of the child and determine the best course of treatment.
Treatment
The key to effective treatment of toe walking is determining the proper combination of treatment techniques for the child, rather than focusing on one, to ensure success. Sensory system deregulation is highly correlated with toe walking and may include deregulation of the tactile (touch), vestibular (balance), and visual (focal and bodily proprioception) systems.
Treatment of a toe walking gait pattern also requires commitment from the patient’s family. Most treatments require long durations to be successful. It is necessary to prepare the family for realistic treatment times and expectations to decrease the likelihood of frustration. Follow-up is essential to successful treatment, as the hours of use and progression of the orthotic device change regularly throughout the course of treatment. Regular follow-up appointments, scheduled every 3-5 months, are recommended. Follow-up appointments are used to gauge any changes in range of motion and frequency.
Stage 1
Patient Profile: Infantile toddler toe walking with no tightness.
Treatment Plan: Attempt to limit plantar flexion and toe extension with orthopedic rigid high-top shoes. Heel lifts can be added to this intervention to ensure the child is getting sensory input through their heel and achieving a foot flat position. Once heel-toe gait is achieved, continue with high-tops in conjunction with an orthotic insert for 1-2 years. The duration of treatment will depend on the amount of time the child has experienced the unaddressed gait pattern.
Stage 2
Patient Profile: 20-30% toe walker and/or weaning off stage 3 or 4 with no tightness, can heel-toe walk when cued.
Treatment Plan: Treatment consists of a combination of a rigid carbon plate, corrective orthotic insert, and high-top shoe, with the possibility of adding heel elevations if needed. This type of treatment may be good for high sensory children when a cast or measurement cannot be achieved for a custom device. It should be utilized as much as possible during the day but may need to be removed at playtime. This treatment should continue for 1-2 years after toe walking is resolved. This level of intervention does not have control over the child’s ankle, so if lower heel walking is noted with early heel rise, and the treatment slows down but does not eliminate the gait abnormality (the child is continuing to toe walk), an ankle-foot orthosis (AFO) intervention may be necessary.
Stage 3
Patient Profile: 30-60% toe walker with no tightness, can voluntarily adapt to heel-to-toe gait when cued.
Treatment Plan: A “toe walking” SMO is a variation of a supramalleolar orthosis with no cut-out for the Achilles tendon and a short extension of the posterior trim line to serve as a kinesthetic reminder during gait to induce proper biomechanics. A full-length foot plate is needed for this design as it better controls the toe extension and lever arms needed to produce a heel-to-toe gait. This toe plate is semi-flexible and does not interfere with the third rocker of gait. The toe walking SMO is an ideal treatment as either an initial treatment or when a child has completed AFO treatment and is weaning down to a less restrictive device.
The SMOs should be worn 6-8 hours per day. The orthoses can be removed for running, playing, and social events. As with most orthotic treatments, SMOs are used for gait training and do not have a positive influence during sitting periods, so children should be encouraged to walk as much as possible when wearing the SMOs. Follow-up appointments should be scheduled every 3 months to monitor progress. If the percentage of time toe walking decreases, the recommended time of use per day decreases in correlation. Once a child has developed a full-time heel-to-toe gait pattern, high-top shoes with orthotic inserts are recommended for 2 years, at minimum.
Stage 4
Patient Profile: 50-100% toe walker with and without tightness.
Treatment Plan: There are many design aspects of solid AFOs that improve the patient’s gait. Appropriate angles are very important to successful outcomes. The success of this treatment option requires that the angle of the ankle in the AFO is appropriate for the patient’s available range of motion. Furthermore, it is always necessary to incline the AFO so the shank to vertical angle is 10-12 degrees with the shoe on, to encourage optimum gait biomechanics.
Determining the length of the calf and footplate section is equally as important to improving gait biomechanics. Children with a toe walking gait pattern typically have underdeveloped foot length, so ground reaction forces in stance are not successful in producing a strong knee extension moment. AFOs should be worn 6-8 hours a day throughout treatment. The child should be seen every 3 months for follow-up appointments and to monitor progress. AFOs should be removed for running, play, and social events. At each follow-up appointment, improvement of the ankle range of motion should be observed before adjusting time in bracing. If there is no improvement, it is recommended to encourage a consult with a therapist to discuss serial casting.
Stage 5
Patient Profile: Children with limited range of motion.
Treatment Plan: If a child has a limited range of motion, a night splint should be worn in combination with the daytime AFOs. Night-time AFOs do not necessarily gain range of motion. They are successful once a good range of motion is comfortable and achieved, and are a good tool to maintain range of motion. A child or an adult will have a hard time sleeping while being stretched, but can comfortably sleep in a maintained position. It is suggested to not start with a nighttime AFO, rather it is a good tool to add after a better range of motion is gained post daytime AFO or casting therapy.
It is essential to differentiate between gastrocnemius and soleus contracture to ensure the correct muscle is on stretch when the child is wearing the brace. If soleus is contracted, an AFO is sufficient. However, if gastrocnemius has a limited range of motion it is necessary to use a knee immobilizer in combination with the AFO. Using orthotic treatment at night time AFO can be difficult, therefore, it is recommended to alternate between right and left every other night to increase compliance. Nighttime splints should be worn for 2 years after heel-to-toe gait has been established to prevent relapse.
Stage 6
Patient Profile: Children with plantar flexion contractures.
Treatment Plan: Serial casting should be considered when a limited range of motion is observed. Serial casting will improve outcomes, gain range of motion, and therefore, decrease the time a child is in treatment. Serial casting proves to be an easy transition into daytime and nighttime AFOs. All children that require serial casting should wear daytime and nighttime AFOs post-casting until the toe walking subsides and nighttime AFOs should be worn for 2 years after heel to gait is established.
Professional Resources
For an overview of treatment, visit:
Sobel E, Caselli MA, Velez Z. Effect of persistent toe walking on ankle equinus. Analysis of 60 idiopathic toe walkers. J Am Podiatr Med Assoc. 1997;87(1):17-22. doi:10.7547/87507315-87-1-17
Caserta AJ, Pacey V, Fahey M, Gray K, Engelbert RH, Williams CM. Interventions for idiopathic toe walking [published online ahead of print, 2019 Oct 6]. Cochrane Database Syst Rev. 2019;10(10):CD012363. doi:10.1002/14651858.CD012363.pub2
Explore Pediatric Event Offerings
Join Hanger Clinic Pediatric Specialists from around the country to continue learning about orthotic and prosthetic solutions for your pediatric patients.
Latest Updates
Subscribe to stay up-to-date on our latest posts.


