ORION 1: Predictors of PROMIS Physical Function in Stroke Survivors Seeking Orthotic Intervention
Journal
Disability and Rehabilitation
Read Online
Download Now
Authors
Sally A. DiBelloa,b, Shane R. Wurdemanc,d, Stacey L. Gorniakaa
- Health and Human Performance, University of Houston, Houston, TX, USA
- School of Health Professions, Baylor College of Medicine, Houston, TX, USA
- Clinical and Scientific Affairs, Hanger Clinic, Austin, TX, USA
- Department of Biomechanics, University of Nebraska, Omaha, NE, USA
Background
Orthotic Research Initiative for Outcomes aNalysis (ORION) 1 is the first of a series of studies aimed at advancing clinical practice and improving outcomes for patients seeking orthotic intervention. ORION 1, conducted by members of the Hanger Institute for Research and Clinical Education, sought to evaluate the functional mobility of adult stroke survivors who use lower limb orthoses.
Objective
Ankle foot orthoses (AFOs) are often used to improve physical function (PF) post-stroke; however, the relationship between the established biomechanical benefits of AFOs and patient perceptions of their mobility has not been fully explored. The purpose of this study was to identify the predictors of self-reported physical function of individuals seeking orthotic intervention post-stroke.
Design (n=237)
Patient Inclusion Criteria:
- Data collected January 2016–June 2020
- 18 years or older
- Diagnosis: stroke
- PROMIS PF collected at initial evaluation
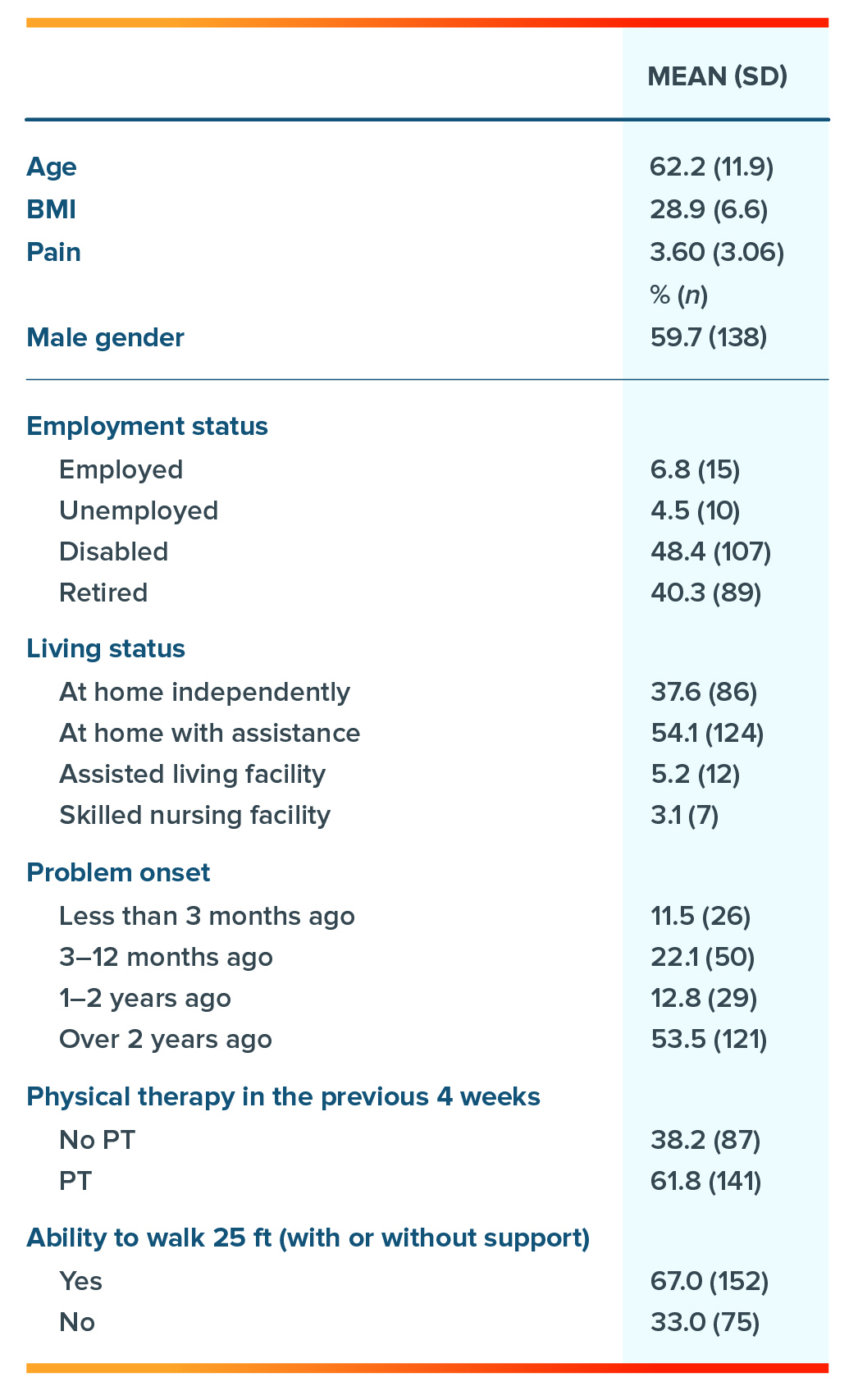
Patient Demographics:
- Mean age = 62.2 (+/- 11.9) years
- Mean BMI = 28.9 (+/-6.6) kg/m2
- Male= 59.7%
- Disabled/retired = 88.7%
- Living with some form of assistance = 62.4%
- Receiving some form of PT = 61.8%
Table 1: Respondent Demographics
Results
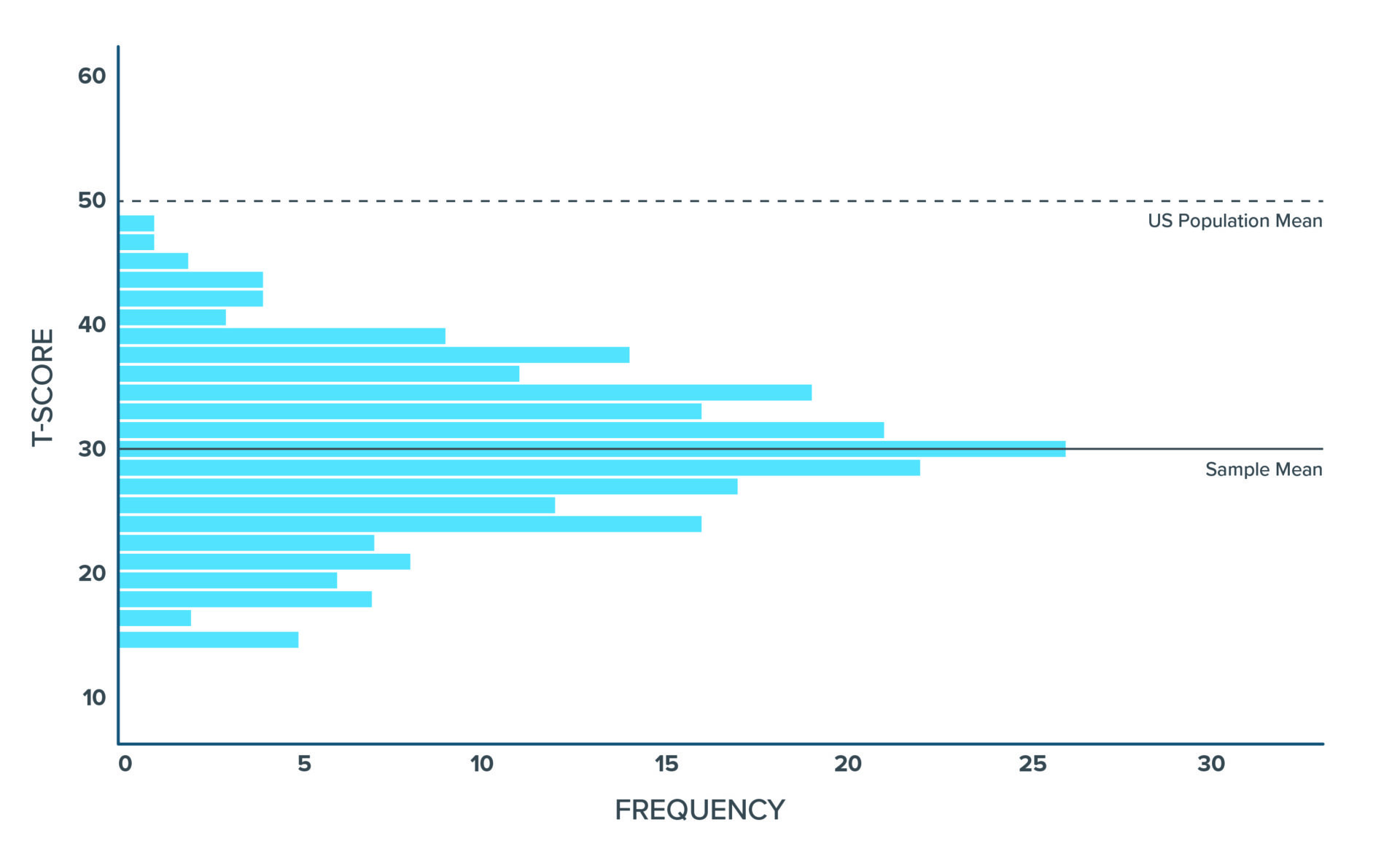
Distribution of T-Score Physical Function for Individuals Seeking AFO Intervention
The mean T-score of physical function of the sample was 30.8, two standard deviations below the U.S. general population mean, demonstrating how physically disabled this population is.
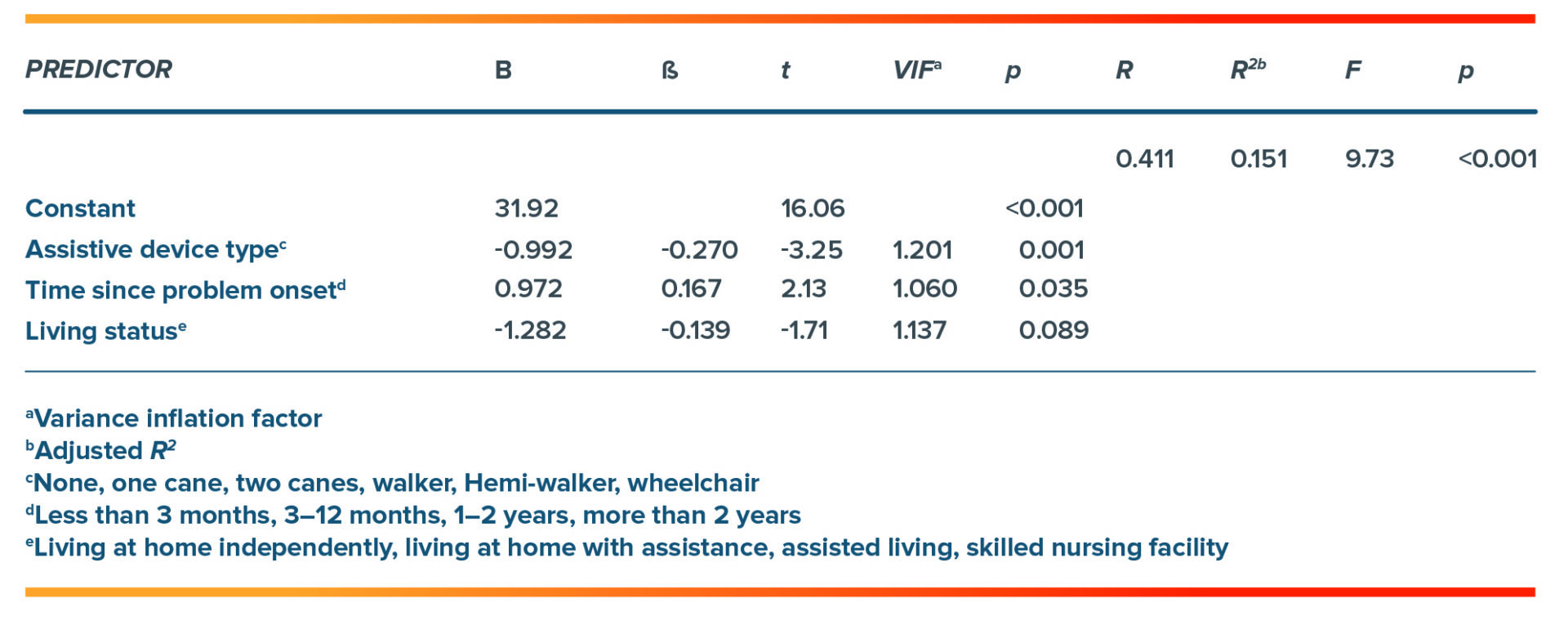
Regression Analysis Summary for Patient-Reported Variables Predicting Physical Function
The regression model explained approximately 15% of the variance in physical function of the sample. Self-reported physical function was worse for individuals requiring more supportive assistive devices, those with more recent ankle problems, and those with greater living assistance.
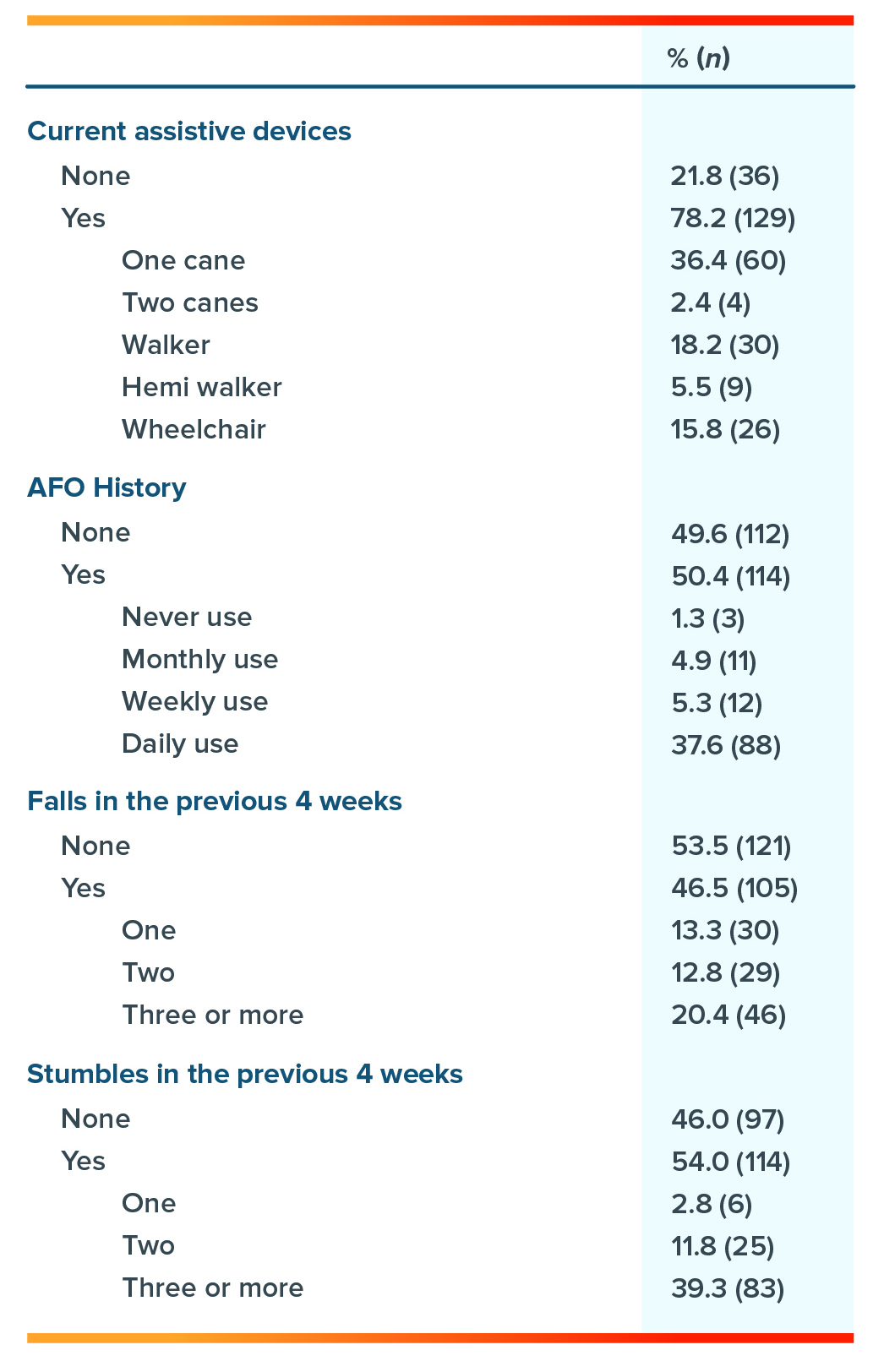
Respondent Device and Fall History
Within this population of stroke survivors, 46.5% reported a fall in the previous month, and 20.4% reported incurring three or more falls during that time. While falls were not a primary analysis, this is novel information surrounding this patient population.
Conclusion
Underscoring the Hanger Institute’s commitment to improving patient outcomes for all patients through leading-edge research, ORION 1 demonstrates the importance of committing resources and time to understanding and advancing clinical practice and improving patient outcomes for users of both orthotic and prosthetic devices.
Specifically, ORION 1:
- Improves our understanding of the factors that contribute to impaired self-reported PF of stroke survivors in need of orthotic intervention.
- Indicates that individuals post-stroke seeking AFO intervention report severe PF impairment.
- Demonstrates that level of assistance, time since ankle and foot problems began, and living assistance status are important clinical characteristics to consider when planning AFO intervention for this population.
- Highlights that AFOs are often used to improve physical performance measures of PF during stroke rehabilitation.
Meet the Authors

Sally A. DiBello, MPO, CPO, LO
Interim Program Director, Orthotics & Prosthetics, Baylor College of Medicine
Ms. DiBello is a leading researcher in the field of lower limb orthotics, seeking to improve patient outcomes through research-driven care.

Shane Wurdeman, PhD, CP, FAAOP (D)
Director, Clinical Research, Hanger Clinic
Dr. Wurdeman has published numerous studies in peer-reviewed journals. In addition to his research work, he continues to manage a patient case load with Hanger Clinic.

Stacy L. Gorniak, PhD
Associate Professor, Department of Health and Human Performance, University of Houston
Dr. Gorniak’s research interests are directed towards evaluating non-traditional movement disorders and how they contribute to long-term disability, particularly with respect to aging, adiposity, and metabolic disorders.
Latest Updates
Subscribe to stay up-to-date on our latest posts.


