Managing Diabetic Foot Complications with the Right Knowledge, Systems, and Support

Chances are you or someone you know – a friend, family member, or co-worker – has been diagnosed with diabetes, a chronic disease affecting over 30 million people in the United States. For Diabetes Awareness Month, we take a look at the importance of proper foot care, prosthetic technology to help those facing limb loss, and the importance of social support.
According to the Centers for Disease Control and Prevention (CDC), diabetes affects over 30 million people, or 9.4% of the population, in the United States.1 If left untreated, it can lead to complications, including heart disease, high blood pressure, stroke, issues with the skin and feet, and potentially even limb loss. In fact, of the nearly 2 million people living with limb loss in the United States, 54% are due to diabetes and peripheral artery disease.2
About Diabetes
There are two types of diabetes – type 1 and type 2.
Type 1 diabetes is not preventable and is often referred to as juvenile diabetes. People with type 1 diabetes cannot produce their own insulin because their body has destroyed the insulin-producing beta cells in the pancreas.
Type 2 diabetes is caused by either the inability to create enough insulin or because the insulin that is being produced isn’t working properly. When insulin isn’t working properly, it is known as insulin resistance. In most cases, type 2 diabetes is frequently developed in those who have a genetic predisposition, have underlying health problems that prevent active and healthy lifestyles, and have adopted an unhealthy diet and eating habits. An estimated 90-95% of people with diabetes have type 2 diabetes.1
Managing Foot Health
If you are experiencing complications with your feet due to diabetes, you are not alone. A large percentage of people with diabetes experience medical issues with their feet.3
Proper diabetic foot care can help you stay active and engaged in your daily activities, and is designed to reduce complications related to diabetes. Your mobility and quality of life depend upon close monitoring of your feet, proper shoe selection, lifestyle choices, and a commitment to your treatment plan.
Additionally, proper foot care can help you avoid problems that may lead to amputation. Practice good hygiene habits by cleansing and thoroughly inspecting your feet and wearing clean socks each day. If you are having trouble healing a wound on your foot, schedule an appointment with your primary care physician or podiatrist to ensure you achieve the best possible outcome.
Custom Diabetic Footwear
Your healthcare team will design a treatment program to meet your needs. Custom inserts, special shoes, and in some cases ankle foot orthoses (AFOs) can be prescribed to take pressure off specific areas of your foot where you struggle to heal and help prevent painful pressure points, blisters, foot ulcers, and sores from developing. They are made to fit your feet and are fabricated from breathable materials designed to cushion while providing extra support to the ankle, arch, and heel.
Diabetes is a complex and debilitating condition, and many people are trying to figure it out on their own. There is a lot of uncertainty in this diagnosis versus many other chronic diseases, and yet look at the ramifications that can come along with it. We need to provide early foot care options and social support to change the shame, the guilt, and the fear that people carry because of this disease.
Leslie Green, Community Care Coordinator
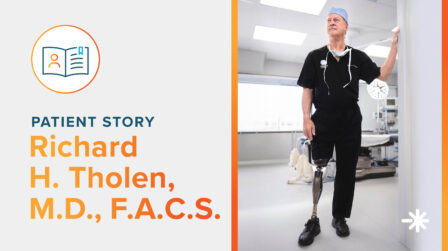
Limb Loss and Diabetes
The cause of amputations in people with diabetes is complex, often resulting from multiple issues in the feet. These may include:
- loss of sensation in the feet from nerve damage (neuropathy)
- poor circulation in the feet from the effects of diabetes on the arteries and small blood vessels
- decreased healing ability and increased risk of infections in the feet and toes

For those facing limb loss, support will be crucial. Leslie Green, Hanger Clinic Community Coordinator, said, “I sit down with individuals with diabetes prior to surgery as they prepare for amputation and the future of walking with a prosthesis. They often feel shame and guilt, like they should have done more. We have to remember this is a chronic disease with so many facets and focus on the next steps. If they still have their other limb, let’s help ensure they are getting support and proper orthotic care to help preserve that limb. We talk through post-surgery expectations, rehabilitation, using prosthetic technology, and how to approach the next chapter in life.”
Post-surgery, wound healing and rehabilitation will be the next steps. You can then work with a Hanger Clinic prosthetist who is trained in the design, fabrication, and fitting of a prosthesis. Research shows that people with diabetes who remain actively engaged in their prosthetic rehabilitation experience high levels of quality of life, satisfaction, and sustained mobility, which is why it is important to talk to your prosthetist about your diabetes and your goals, expectations, and concerns so he or she can address your specific needs.4
Ongoing Diabetes Care
Leslie Green also shared how important it is to have a support system.
“Social and family support are some of the most influential and important factors to successfully control diabetes. Diabetes is a chronic disease that requires extensive behavioral changes and adherence to a complex diet. Additionally, diabetics often face other underlying health issues impacting their life.
In addition to social support, education and a medical support team also play a vital role. Your Hanger Clinic pedorthist, orthotist, or prosthetist is just one member of your team. Other team members may include your family doctor, rehabilitation consultant, diabetes educator, podiatrist, physiotherapist, and pharmacist. The team may grow to include a dietitian, a psychologist, and an occupational therapist. It can seem overwhelming at times, however, a team approach is the best way to manage long-term wellbeing. Managing diabetes can be quite complex but with systems in place to support your needs, you can learn what to do and have access to care when you need it.”
Balanced with Diabetes
Interested in more information about living with limb loss and diabetes? Reach out to Leslie Green to connect with others and get information about education, resources, and community.
Email: [email protected]
Request a Free Evaluation
If you or someone you love is looking for personalized diabetes foot care, contact our Customer Care Center to find a Hanger Clinic footwear location near you.
References
[1] National Diabetes Statistics Report, 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes-stat-report.html
[2] Ziegler‐Graham, et al. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Archives of Physical Medicine and Rehabilitation 2008;89(3):422‐9.
[3] Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther. 2008;88(11):1254-1264.
[4] Wurdeman S, Stevens P, Campbell J. Mobility Analysis of AmpuTees (MAAT 6): Mobility, Satisfaction, and Quality of Life among Long-Term Dysvascular/Diabetic Prosthesis Users—Results of a Cross-Sectional Analysis. Journal of Prosthetics and Orthotics 2021;33(3):161-167.
Latest Updates
Subscribe to stay up-to-date on our latest posts.