Mobility Analysis of AmpuTees (MAAT VI): Mobility, Satisfaction, and Quality of Life among Long-Term Dysvascular/Diabetic Prosthesis Users—Results of a Cross-Sectional Analysis
Journal
Journal of Prosthetics and Orthotics
Read Online
Download Now
Authors
Shane R. Wurdeman, PhD, CP, FAAOP(D)1,2, Phillip M. Stevens, MEd, CPO, FAAOP1,3, James H. Campbell, PhD, CO, FAAOP1
- Department of Clinical and Scientific Affairs, Hanger Clinic, Austin, TX
- Department of Biomechanics, University of Nebraska at Omaha, Omaha, NE
- School of Medicine, University of Utah, Salt Lake City, UT
Background
Though many major lower-limb amputations may result from traumatic injury or acute disease processes such as cancer or septic infection, the most common cause in the United States is vascular disease typically associated with diabetes. Recent literature on the long-term prognosis of individuals who undergo major lower-limb amputation as a result of vascular disease and diabetes highlights significant mortality rates in the years following the procedure. Long-term mobility levels among individuals with amputation due to vascular disease have generally been reported in a binary fashion, distinguishing only between those who sustain or lose their ability to walk. The objective of this study was to illustrate the quality of life, satisfaction, and mobility of those with amputation due to vascular disease and/or diabetes that continue to maintain their prosthetic care.
Objective
To establish the mobility, satisfaction, and quality of life (QoL) among prosthesis users with dysvascular/diabetic amputation at both acute and long-term phases of prosthetic rehabilitation.
Design
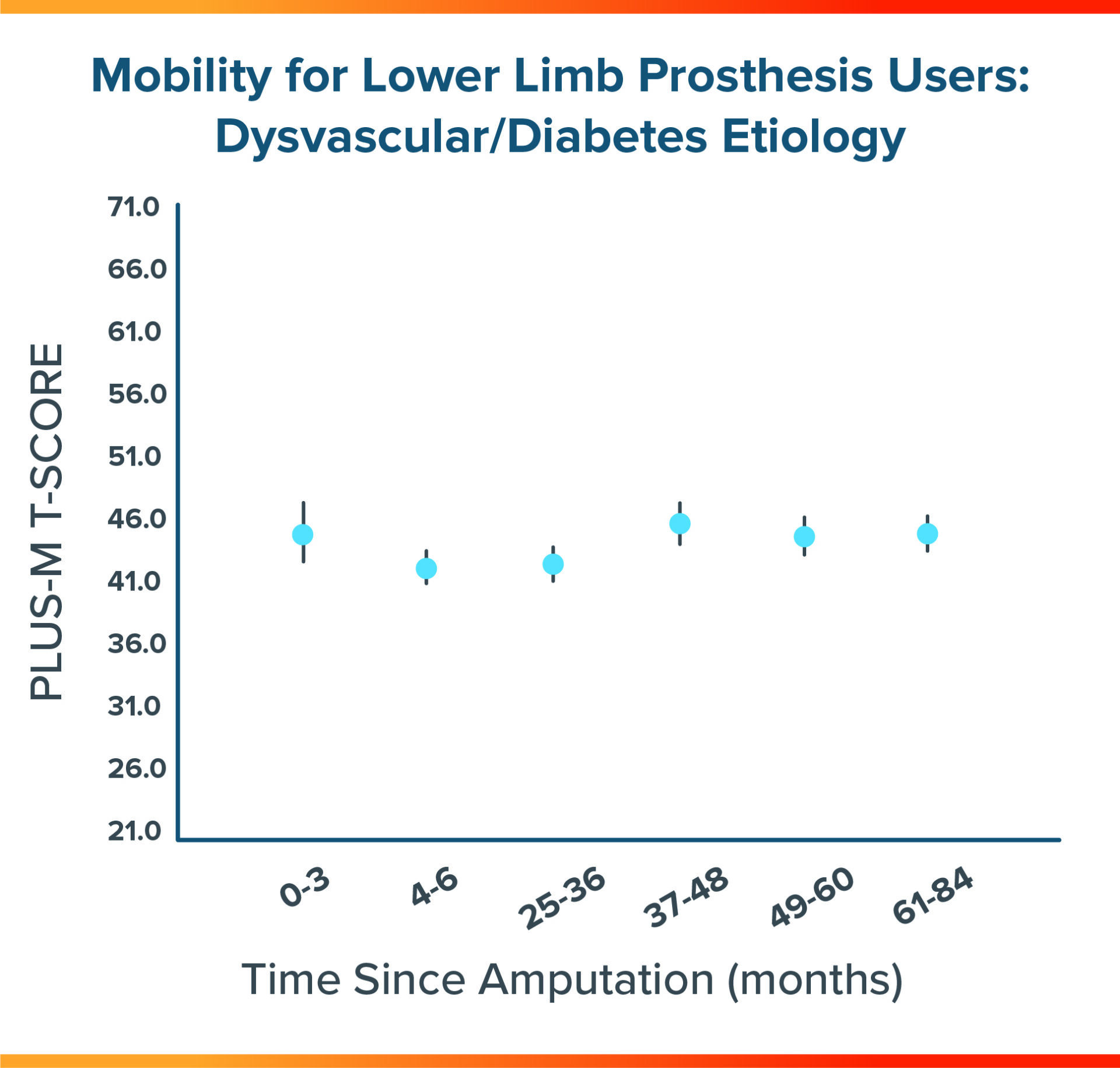
A total of 341 individuals met the inclusion criteria and were included in the final sample of this cross-sectional analysis. Patients were grouped into acute phases (0-3 months, 4-6 months) and chronic phases (24-36 months, 37-48 months, 49-60 months, and 60-84 months) after amputation. Mobility was measured with the Prosthetic Limb Users Survey of Mobility (PLUS-M), whereas QoL and satisfaction (Sat) were reported using 10-point scales adapted from the Prosthesis Evaluation Questionnaire — Well-Being (PEQ-WB). Group differences were compared using separate general linear univariate models.
Results
FIGURE 1
Sat values for patients 0 to 3 months postamputation were significantly higher than Sat values observed in cohorts 25 to 26 months, 49 to 60 months, and 61 to 84 months postamputation. Similarly, the highest QoL values were observed in those individuals 0 to 3 months postamputation. Otherwise, there were no significant group differences across acute and chronic cohorts for mobility, PEQ-WB, or QoL.
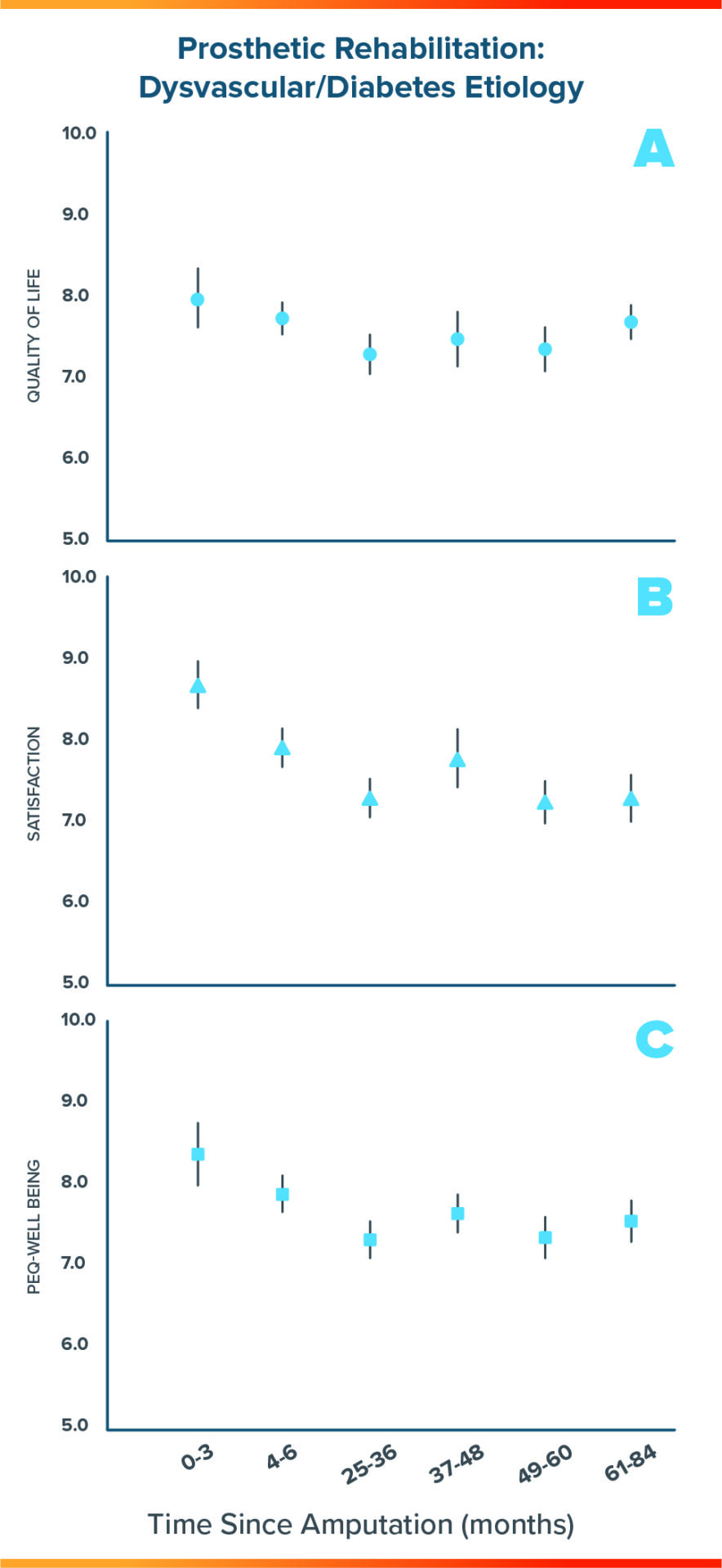
Figure 2
Among acute users of lower-limb prostheses, the highest QoL values were observed among individuals 0 to 3 months postamputation. Among long-term users, the highest QoL values were observed among individuals 61 to 84 months postamputation.
Conclusion
- Patients with vascular disease or diabetes who remained engaged in prosthetic rehabilitation as far out as 7 years post-amputation experienced high levels of quality of life, satisfaction, and sustained mobility.
- Integration of continued prosthetic rehabilitation into the post-amputation care plan as well as sustained utilization of a prosthesis can help patients thrive, which is critical in light of elevated mortality rates observed in this population.
Meet the Authors



More Published Research
This publication is just one of the studies conducted by the Hanger Institute for Clinical Research and Education, in collaboration with leading researchers, clinical, and academic institutions.
Latest Updates
Subscribe to stay up-to-date on our latest posts.