IMPACT 2: The Role of Earlier Receipt of a Lower Limb Prosthesis on Emergency Department Utilization
Journal
PM&R Journal
Read Online
Authors
Taavy A Miller, MSPO1,2, Rajib Paul1, PhD, Melinda Forthofer, PhD1, Shane R. Wurdeman, PhD2,3
- Department of Public Health, University of North Carolina at Charlotte, Charlotte, NC, USA
- Department of Clinical and Scientific Affairs, Hanger Clinic, Austin, TX, USA
- Department of Biomechanics, University of Nebraska at Omaha, Omaha, NE, USA
Background
In order to quantify the impact on healthcare utilization, emergency department utilization was applied as a proxy for overall healthcare utilization. Two separate models were implemented to determine associations to utilization. The first model evaluated the effect of timing of prosthesis receipt on utilization. The second model assessed the impact adverse events (i.e. falls or fractures) had on utilization within this unique population.
Objective
To determine the role timing of prosthesis receipt has in emergency department (ED) utilization and the association of fall/fall-related injury with healthcare utilization.
Design
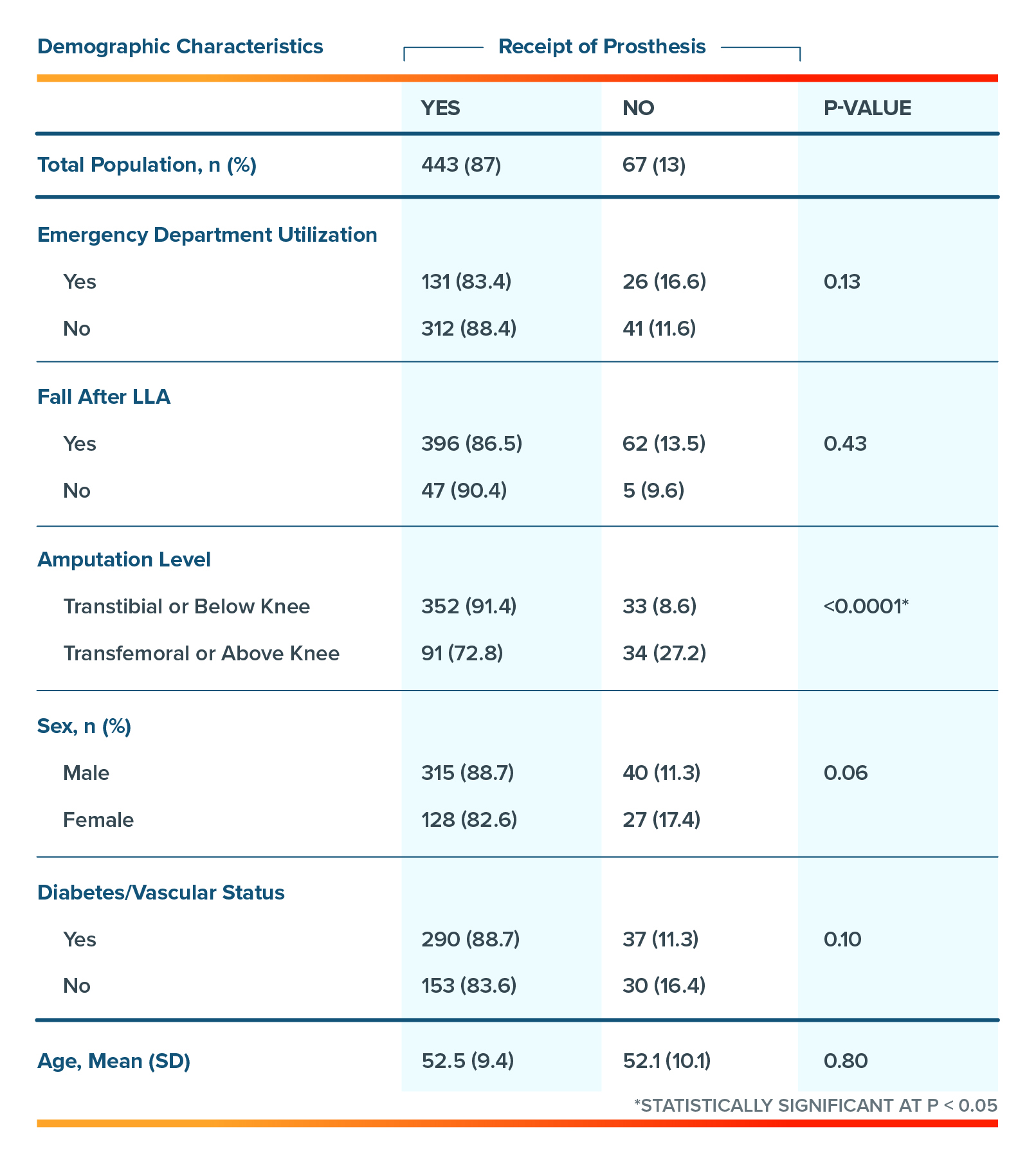
Data on adults with lower limb amputation (n=510) were obtained from a nationally representative administrative claims database (Watson). All individuals were continually enrolled on a commercial insurance plan for the entirety of the period from 2014-2016.
About Watson: The Watson database is a large US private sector health claims database containing de-identified records representing approximately 25% of all commercial claims aggregated into one database with patient-level enrollment history, medical, and pharmacy commercials claims nationwide.
Patient Inclusion Criteria:
- Lower limb amputation
- Continually insured for the 3-year period
Patient Demographics:
- Between ages of 18 – 64
- 75% had a Transtibial amputation (p<0.0001)
- 70% were male (p=0.06)
- 64% were diabetic or had vascular disease (p=0.11)
- Average age: 52 years (± 9.4 years)
Table 1: Sample demographic characteristics and inferential statistics stratified by receipt of prosthesis.
Results
- Individuals who received a prosthesis early, within 0 to 3 months, post-lower limb amputation were 48% (OR=0.52 95% CI: 0.28 – 0.97) less likely to use the emergency department (ED) compared to those who did not receive a prosthesis across all age groups.
- The percentage of ED use as a measure of overall healthcare utilization, appears to have an upward trend as the time from surgery to prosthesis receipt increases (figure 2).
- Individuals who experienced a fall/fx had 2.8 (OR=2.86 95% CI: [1.23-6.66]) times the odds of ED utilization.
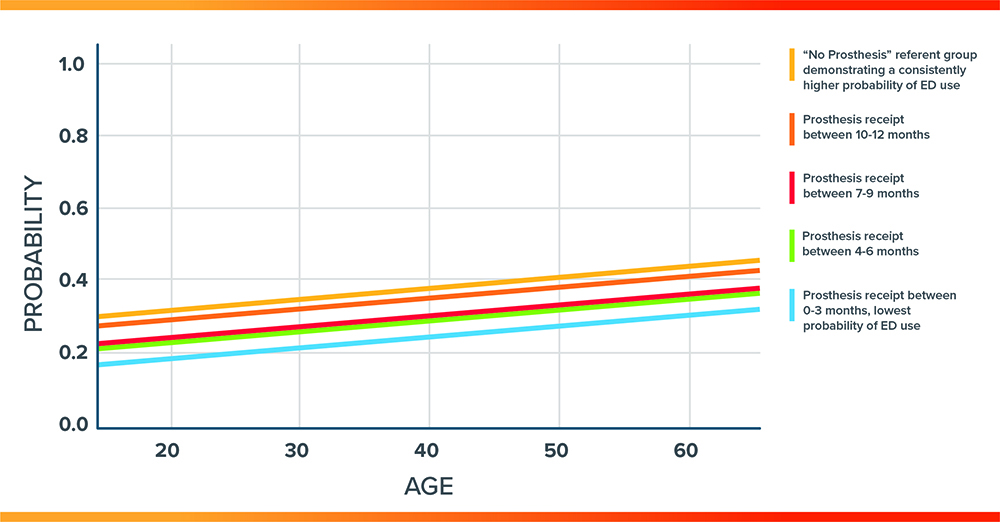
- The predicted probability of healthcare utilization across all ages stratified by timing of prosthesis receipt also visually demonstrates the increased utilization as prosthesis receipt is delayed or no prosthesis within 12 months (figure 3).
Figure 2: Comparison of percent of emergency department (ED) use that changes based on timing of prosthesis receipt proportional to group size
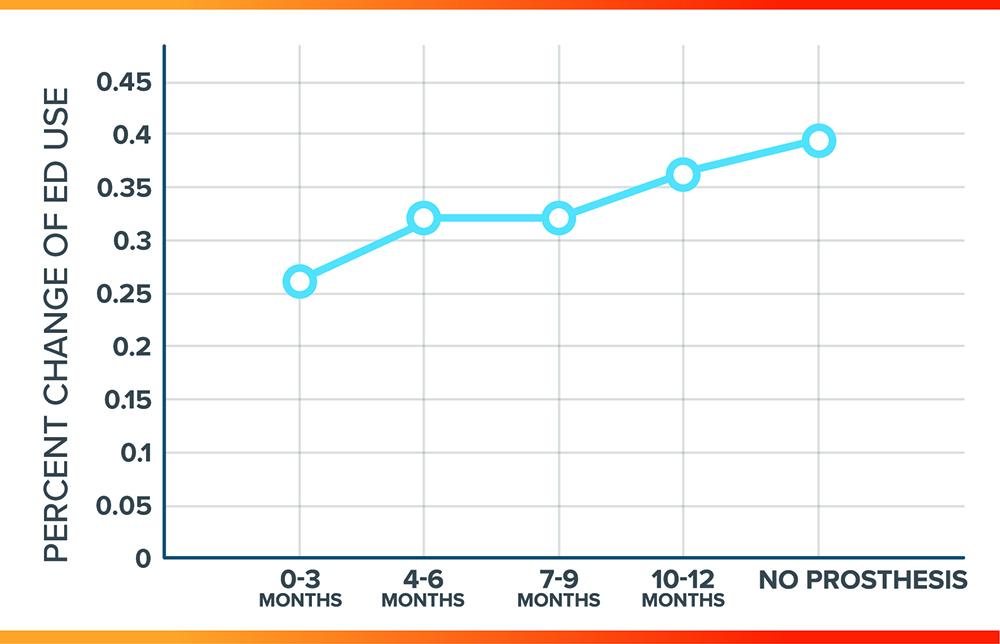
Figure 3: Predicted probability of ED use versus age stratified by time to prosthesis receipt
Conclusion
- Receipt of a prosthesis reduces the risk of emergency department use and therefore may reduce overall healthcare utilization.
- If an individual is provided a prosthesis earlier in the rehabilitation process after lower limb amputation, there is increased value and opportunity to avoid preventable healthcare utilization and further reductions in quality of life.
- Occurrence of adverse events, i.e. fractures and falls, are drivers of increased healthcare utilization, as opposed to chronic health issues.
- The current study underscores the value of prostheses during the rehabilitation process after lower limb amputation.
Authors from Hanger Clinic

Shane Wurdeman, PhD, CP, FAAOP (D)
Director, Clinical Research, Hanger Clinic
Dr. Wurdeman has published numerous studies in peer-reviewed journals. In addition to his research work, he continues to manage a patient case load with Hanger Clinic.

Taavy A. Miller, PhD, CPO
Research Scientist
After earning her MSPO and working as a CPO, Taavy taught O&P and then earned her PhD in health services research. She has published several studies in peer-reviewed journals, presented abstracts at various conferences, and currently works as a research scientist conducting and leading research projects with a focus on patient outcomes.
Latest Updates
Subscribe to stay up-to-date on our latest posts.