Using Data to Improve Prosthetic Patient Outcomes

While there have previously been small-scale efforts within prosthetics rehabilitation to measure outcomes, many involved instruments that were far too time-consuming for the clinic setting. While the instruments evolved over time and became easier to use, a solution for implementation remained unclear.
Because Hanger Clinic sees more prosthetic patients than any other organization in the world, we felt it was our responsibility to help refine and further develop a tool that could easily be integrated into the clinical care pathway and shared with patients on an ongoing basis.
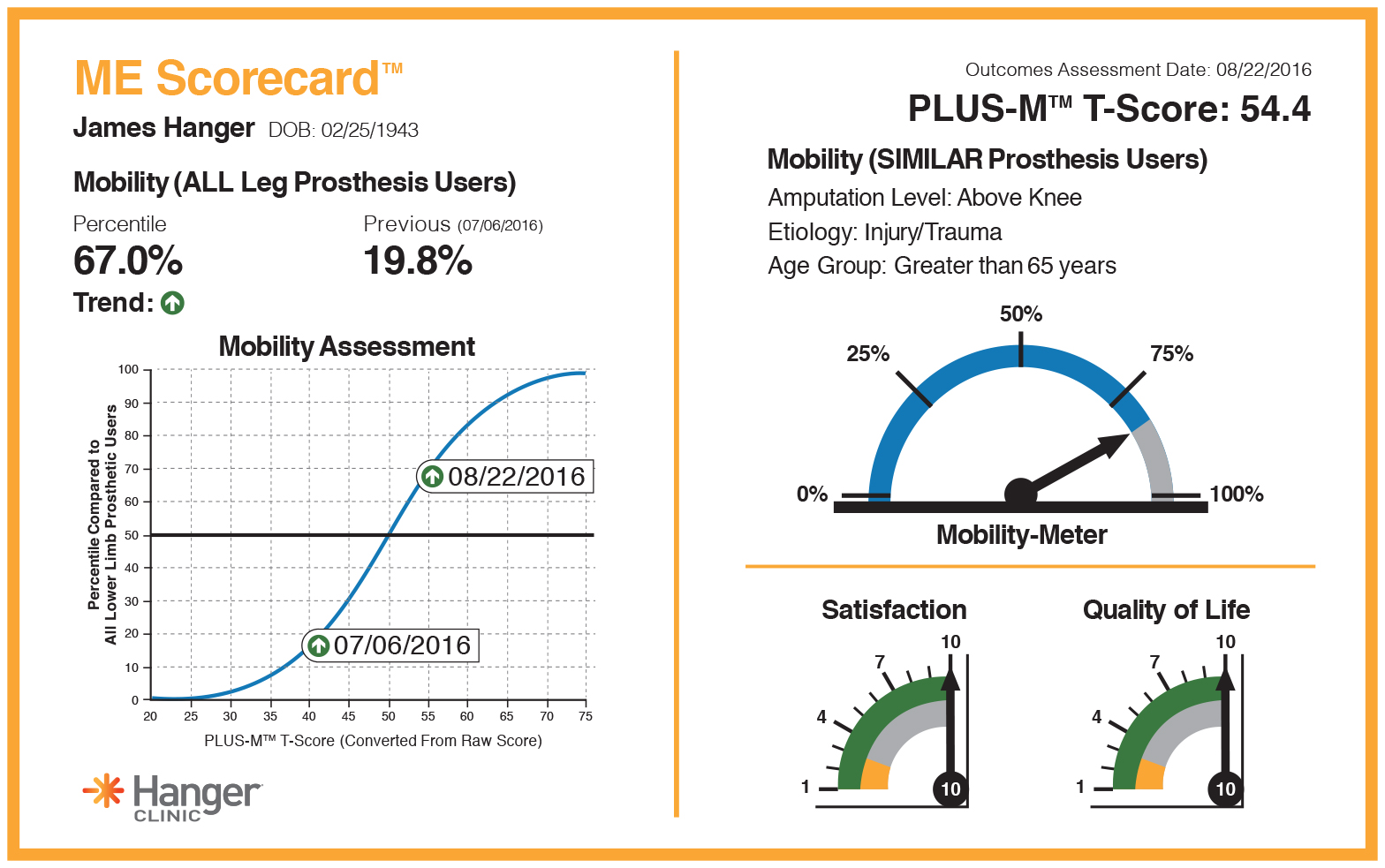
The result of our efforts is a new clinical outcomes protocol, called ME™ by Hanger Clinic, that consists of the PLUS-M™ (Prosthetic Limb Users Survey of Mobility) and Mobility Empowerment (ME) Scorecard™.
The PLUS-M quantifies and records how well lower extremity prosthetic patients are doing. It was developed by Dr. Brian Hafner at the University of Washington through a National Institutes of Health (NIH) grant.
PLUS-M may be a more accurate measure of a patient’s ability because it’s not just the clinician observing the patient in a gait lab. It is unique in that it’s a survey prosthetic patients complete themselves. It asks them to answer questions about their mobility in everyday situations, from walking a short distance indoors to hiking long distances on uneven ground. It also asks them to rate the degree of difficulty when engaged in various activities from “unable to do” to “without any difficulty.”
When the patient completes the PLUS-M instrument, his or her clinician is provided with the proprietary scorecard, which provides information specific to the patient’s progress, including satisfaction, quality of life, and mobility. The patient’s mobility is given as a benchmark relative to the general population of lower limb prosthesis users, as well as those patients with similar etiology, age, and amputation level.
Other than tracking individual patient progress, outcomes are also being used by Hanger Clinic’s Department of Clinical and Scientific Affairs to report population outcomes. Because we have the ability to aggregate the outcomes data collected by patients at volumes never before reported, we can shed light on aspects of prosthetic rehabilitation that were previously not known or possibly reported on sample sizes that were too small to provide strong answers. For example, we recently conducted an analysis on nearly 600 patients with a lower limb prosthesis and found that co-morbidities do not impact lower limb prosthesis users’ mobility to the degree previously believed. Information like this can begin to change misperceptions about patients with co-morbidities—misperceptions that may have previously improperly informed a clinician’s plan of care.
Benefits to Patients, Clinicians, and Payers
The ME Scorecard™ helps clinicians and patients understand how well the patient is doing while being benchmarked against their peers. As a result, it is possible to know and realize if a patient is truly reaching their potential or if there should be a change in the current plan of care.
The patient also benefits because they are empowered to understand and participate in their own care, which can lead to higher satisfaction. And, when a patient is able to see they are doing above average, it helps improve confidence, self-efficacy, and overall understanding of their care.
The scorecard–it makes you sit back and think, but also at the same time, it makes you give yourself a pat on the back. It really gives confirmation that everything you’re doing is for the right reasons. It’s proving, physically, that you’re doing better.
Lynne C., Hanger Clinic patient
Enhanced Information for Physicians
By recording patient outcomes, patients and clinicians have the ability to better gauge the patient’s potential, which can help the entire rehabilitation team improve care.
Physicians involved with amputee rehabilitation now have the ability to see an objective, quantified measure of their patients as they go through rehabilitation. In many other areas of care, physicians are able to assess their patients and track progress to help determine whether a change in the current plan of care is necessary. Now, this will be possible for physicians involved with amputee care.
In my practice, I am able to pick the outcome measurement tools that are most appropriate for the patients’ diagnosis, [and] I’m excited to add this [scorecard to the repertoire to show patients how they are doing in a more effective format.
Amy Stone, PT, DPT, GCS, CWS, CLWT
The Next Step
As part of the development process for PLUS-M, data was collected on ~1100 patients with lower limb amputations. The instrument is currently being used at select Hanger Clinic locations and will continue to be refined and improved by its developers. To assist in this effort, we entered into a license agreement with the University of Washington where we will use the PLUS-M instrument to help our prosthetists monitor patient mobility, and in turn, de-identified data that is collected for clinical purposes will be provided back to them.
Latest Updates
Subscribe to stay up-to-date on our latest posts.