OASIS 2: Mobility Differences with Specific Prosthetic Feet Across Procedure Codes
Journal
Journal of Rehabilitation and Assistive Technologies Engineering
Read Online
Download Now
Authors
Taavy A. Miller, PhD1,2, James H. Campbell, PhD1, Dwiesha L. England, MS 1, Phillip M. Stevens, MEd1,3, Shane R. Wurdeman, PhD1
- Hanger Institute for Clinical Research and Education, Austin, TX, USA
- School of Health and Rehabilitation Sciences, University of Pittsburgh, Pittsburgh, PA, USA
- School Division of Physical Medicine and Rehabilitation, University of Utah Health, Salt Lake City, UT, USA
Background
The prosthetic foot is a unique tool provided to patients as part of their overall prosthetic rehabilitation following limb loss. There is a category of prosthetic foot in particular, coded as L5987, which was predicted to enable higher functionality by integrating vertical shock absorption. Originally, this functionality was achieved through additional mechanical components attached to the foot, adding both build height and weight. However, improvements in geometries and materials science allowed these feet to evolve to the point that they could potentially provide similar functional benefit without the added weight and height of the visible vertical shock absorption units.
Recently, the organization that assigns prosthetic components their categorical codes (PDAC) re-classified several L5987 feet to an L5981 code due to the lack of an obvious, visible additional vertical shock absorption unit. This was done without consideration for the performance or observed function of the feet. Rather, the decision was informed by the presence of distinct mechanical features.
The purpose of Outcomes ASsessment and DISsemination (OASIS) 2 was to compare patient-reported functional mobility across a range of prosthetic feet using real-world clinical outcomes data. It is the second study in the OASIS series by the Hanger Institute for Clinical Research and Education comparing the effectiveness of prosthetic components across patient groups to impact and enhance patient outcomes.
Learn more about OASIS 1, which compared outcomes from four common microprocessor knee models.
Objective
To investigate real-world evidence on several highly utilized prosthetic feet that were re-coded from L5987 to L5981 due to a lack of a visual distinct vertical loading mechanism.
Design (n=526)
A retrospective, observational review of patient outcomes data was completed to assess mobility across foot categories and between different prosthetic feet coded as L5987 or L5981.
Patient Inclusion Criteria:
- Data collected from January 2016-December 2021
- 18 years or older
- Major lower limb amputation (i.e. transtibial, knee disarticulation, or transfemoral)
- Currently using a prosthesis
- Completed mobility outcomes after confirmed delivery of a new prosthetic foot
Patient Demographics:
- Average age = 52.5
- 83% Male
- 78% Transibital amputation
- 37.4% Vascular disease / diabetes
- 27% Trauma
- 35.6% Cancer, congenital, and / or not reported
- K3 Ambulators = 523
Patient Foot-Type Groups:
- Sustained-87: Prosthetic feet which underwent recent PDAC review and remained coded as L5987 base code
- Modified: Prosthetic feet which were previously considered within the field with the L5987 base code but as of 1 January 2021 are PDAC recommended for L5981
- Not Reviewed: Prosthetic feet which have not yet been submitted for PDAC review
- Original-81 (Control Group): Prosthetic feet that have previously been reviewed by PDAC and assigned code L5981
Research Short: An Overview of OASIS 2
Hear the perspective of two OASIS 2 study authors, Phil Stevens, MEd, CPO, FAAOP, and Shane Wurdeman, PhD, CP, FAAOP(D), as they provide insight and clarity into the objectives and findings of OASIS 2.
Results
The results showed L5987 feet had greater functional mobility than the Original-81 feet. There was no significant difference in functional mobility for individuals with prosthetic feet that had their coding modified to L5981, compared to those that retained the L5987 designation.
FIGURE 1
Category Comparison
Post hoc analysis showed the Sustained 87 category to be significantly greater than the Original 81 category (P<.0001). Notably, there were no statistical differences between the Sustained 87 and Modified categories (p=.55) or between the Modified and Not Reviewed (p=.62).
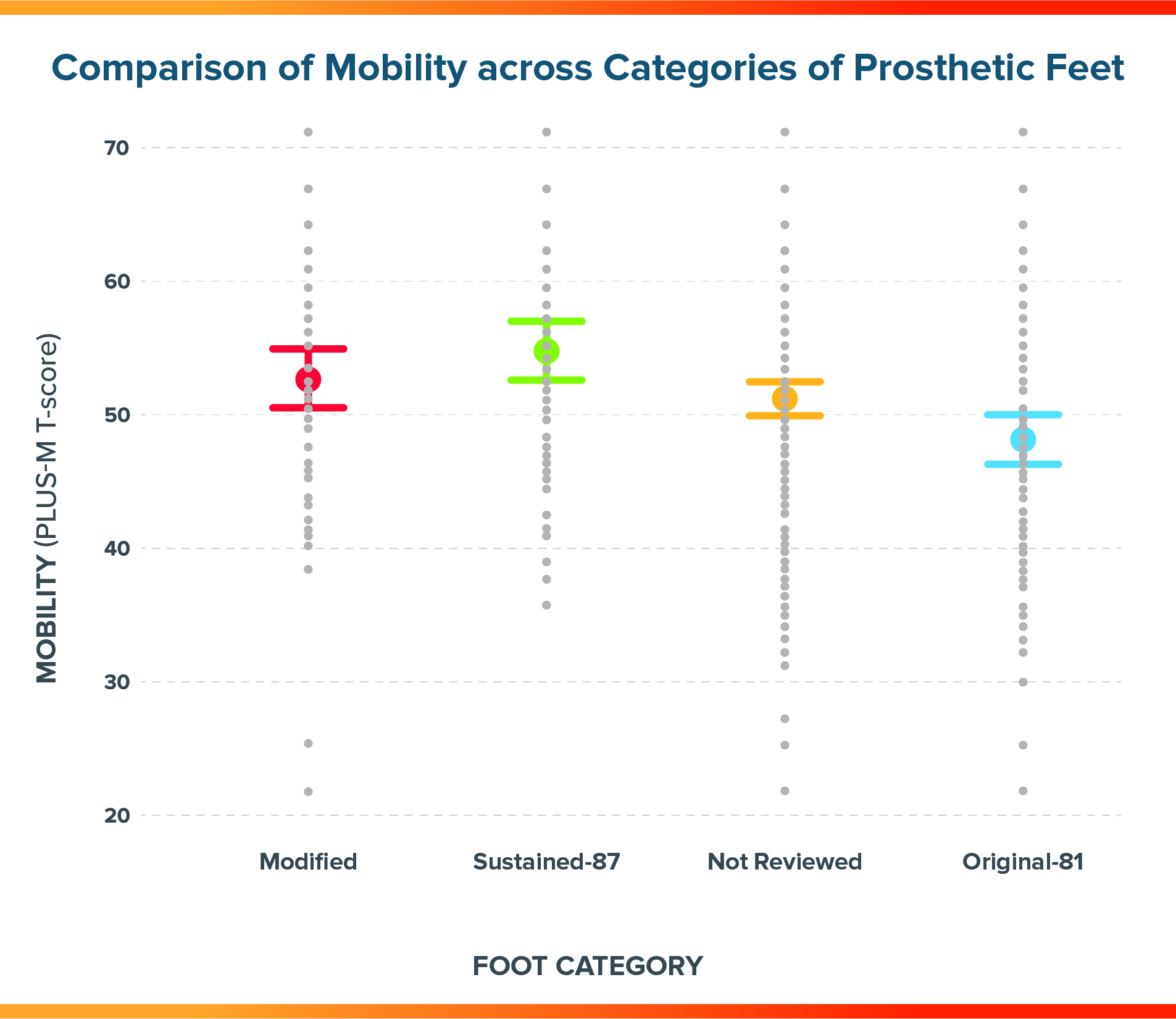
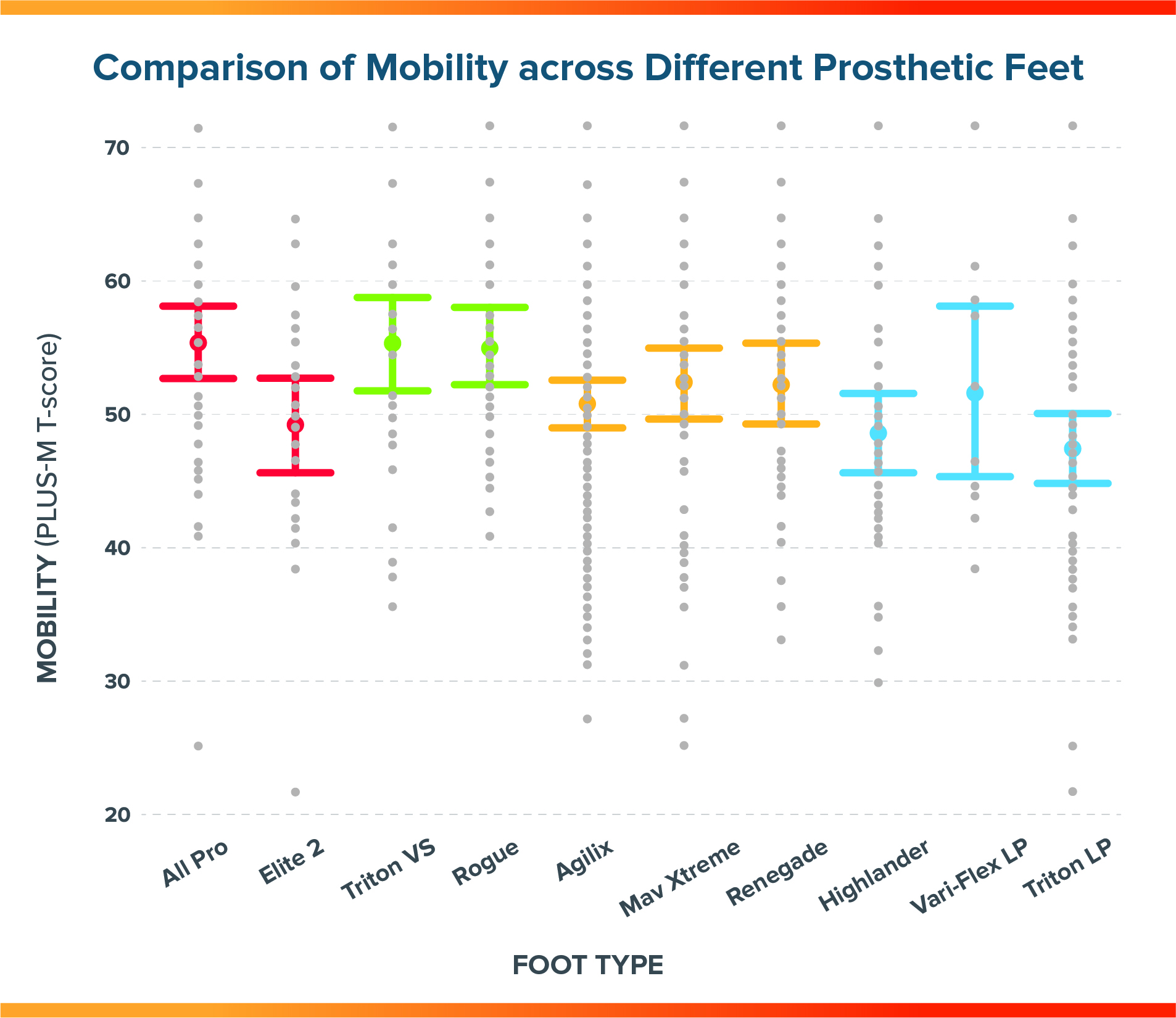
FIGURE 2
Mobility Comparison
Specific make and model of feet within each category performed fairly consistently although there were exceptions.
- The Fillauer All Pro within the Modified category performed similarly to the feet within the Sustained 87 category and seemed to overall increase the average performance of the feet grouped in the Modified category.
- The Ossur Vari Flex LP, although there was large variability, seems to be performing better than the other feet within the Original 81 category.
Conclusion
- The study of 526 individuals with a lower limb prosthesis showed that L5987-coded feet are associated with improved mobility compared to the L5981 category, a confirmation of results reported previously in a purely dysvascular/diabetic population of 738 individuals with amputation in the Institute’s Mobility Analysis of Amputees (MAAT) 5 study.
- The real-world clinical outcomes data evaluated in this study emphasizes functional performance over visible characteristics as a pathway toward higher performance for the end user.
- Having the ability to objectively measure, analyze, and disseminate real-world functional outcomes enables clinical providers to make informed, unbiased decisions about patient care, resulting in enhanced outcomes.
Meet the OASIS 2 Authors




More Published Research
The OASIS series is part of a vast collection of landmark research studies already published, or in various stages of publication by the Hanger Institute for Clinical Research and Education, in collaboration with leading researchers, clinical, and academic institutions.
Latest Updates
Subscribe to stay up-to-date on our latest posts.


